Happy May!
First of all, I’d like to congratulate Anderson Cooper on the birth of his son, Wyatt Morgan Cooper. Among this never-ending heartbreaking news cycle, it’s nice to have a little joy. In a strange turn of events, a tweet I posted about the baby’s birth went viral, with over 110,000 impressions on Twitter.
It’s Week 3 in my weekly report on my recent reading on the Covid-19 pandemic and how I see some possible ways going forward. You can read the first report here and the second one here. Again, I’m not a public health expert — just a student journalist who has been monitoring this crisis since I was caught in the middle of the initial outbreak in China. Like last week, we’ll be focusing on three major topics: a national view, higher education and study abroad.
In the words of Chris Cuomo, “Let’s get after it.”
A national look
A major contradiction exists in our nation. A few weeks ago, the White House released guidelines stipulating that states should wait for a 14-day decline in coronavirus cases before moving to the next phase of lifting some restrictions. It seems like no state has waited to achieve this metric, with over 26 states opening some form of their economies at the end of this week. This has led to contradicting efforts on states, counties and even municipalities to defy orders from the higher levels of government — for example, while Colorado is lifting restrictions, Denver is maintaining its stay-at-home order. As a geographer, this conflict across geographic scales puzzles me. This did not exist in China’s response — it was all a top-down approach.
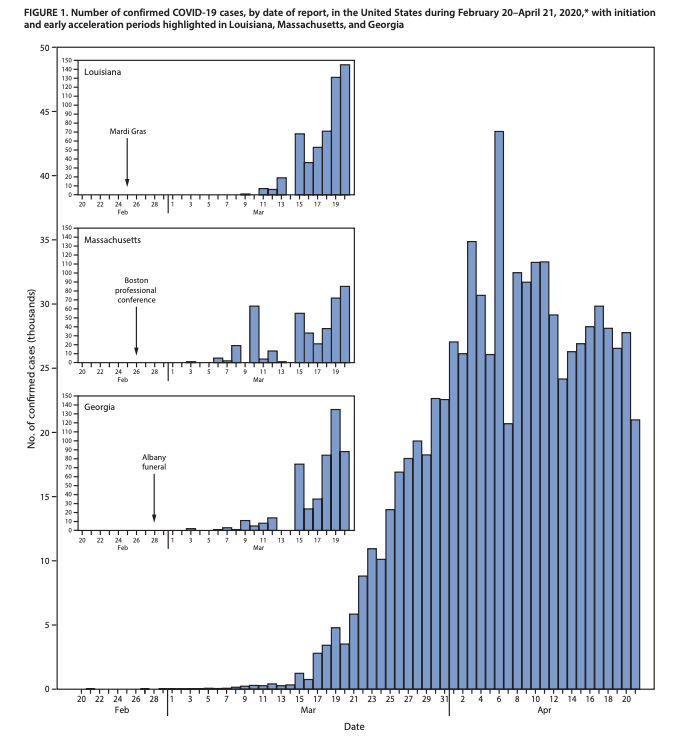
Let’s start today’s discussion with a new report released on May 1 by the CDC detailing the factors that contributed to the accelerated speed of the coronavirus in the United States. These factors are:
- Continued travel-associated importations of the virus
- Large gatherings (Mardi Gras, the biotech conference in Boston, etc.)
- Introduction of the virus into high-risk areas (nursing homes, dense populations)
- Challenges in detection (limited testing and the overlap with flu season)
The report is interesting in itself to read, but I wanted to highlight one point:
“After Chinese authorities halted travel from Wuhan and other cities in Hubei Province on January 23, followed by U.S. restrictions on non-U.S. travelers from China issued on January 31 (effective February 2), air passenger journeys from China decreased 86%, from 505,560 in January to 70,072 in February. However, during February, 139,305 travelers arrived from Italy and 1.74 million from all Schengen countries,* where the outbreak was spreading widely and rapidly.”
This contributes to the growing body of evidence that while the travel restrictions from China helped, the European transmission of the virus had a huge effect on community spread in the United States. Global travel has doubled since the last pandemic in 2009. In addition, large events such as Mari Gras, a professional conference in Boston and a funeral in Georgia serve as examples of areas that accelerated the spread of the virus.
When opening a state’s economy, authorities are monitoring three main factors, according to New York Governor Andrew Cuomo:
- Number of hospitalizations
- Number of positive diagnostic tests
- Number of positive antibody tests
These metrics are key to get a glimpse of how a state is progressing in the handling of an outbreak. We are still seeing over 1,000 Americans lose their lives nationwide each day. In my opinion, we are in no place to let up now.
Let’s unpack what these tests do for us. This is not a cookie-cutter virus. It affects everyone differently. At around a 10% hospitalization rate (based on previous data), we must account for those who do not end up in the hospital and recover at home. These numbers of patients with mild to moderate symptoms (who do not end up in the hospital) must be closely monitored.
This week, the CDC broadened the list of symptoms to include:
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
These new symptoms are in addition to fever, cough and difficulty breathing. This could increase the number of cases as we increase capacity of testing.
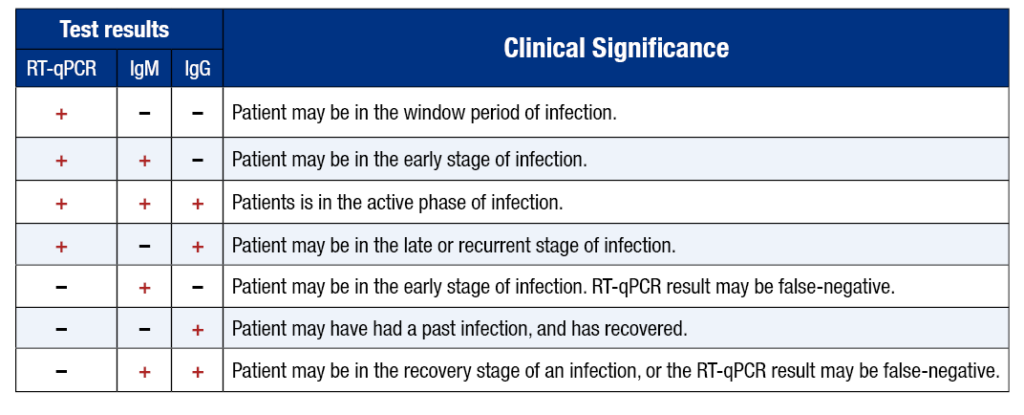
Let’s talk about diagnostic tests. We need more of them. But we also must be mindful that they are not all accurate and false negatives can be up to 15%. A positive rate of around 10% is critical to show the spread and an accurate level of surveillance. With more testing, we can determine the spread of this outbreak. Just look at Rhode Island (left) vs. New York (right) test results. Rhode Island has tested 5% of its population, compared to New York, who until recently had only tested the sickest. Rhode Island’s age distribution is much more even compared to New York’s. This is because the oldest and the most vulnerable are the ones going into the hospitals and getting tested.


We also need to know the ones who are getting sick as the country has been in social distancing measures for over 6 weeks. Are these essential workers who are already exposed? Are there other pockets we don’t know about? In some states where there are small amounts of cases, this influx in cases could represent a reality check more than a surge — it lets us know what we’re up against.
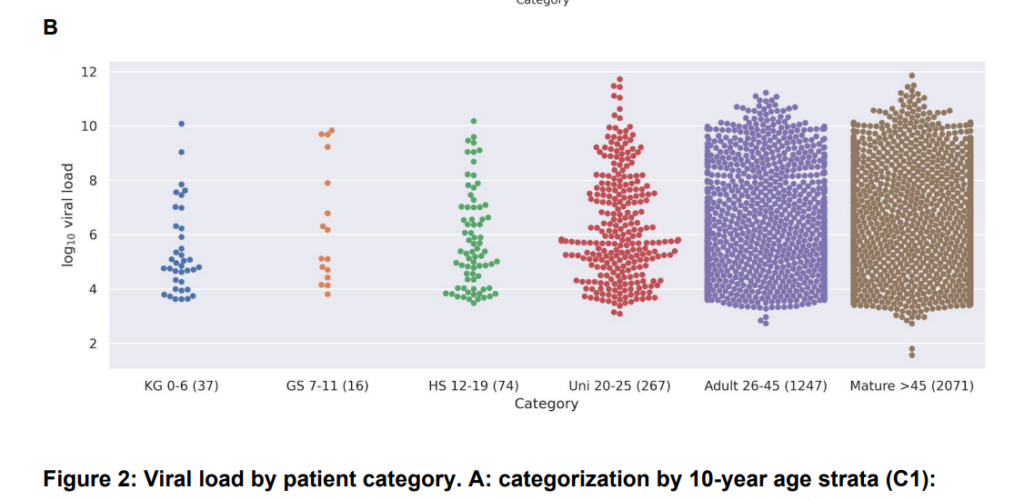
This pandemic is confusing and we need to understand more. A German study shows that children shed around the same viral load as adults and thus they may be just as infectious. Studies in areas such as nursing homes and hospitals are so vital to understand how people are getting sick. This is clearly more fatal than the flu (just in case Sean Hannity is reading this and still doesn’t believe science).
I would like to talk about transmission. Currently, the extent of the knowledge and research is that the virus is mainly transmitted through respiratory droplets and close contact (like this cluster in Singapore). This does not mean that it cannot be transmitted through the airborne route, as seen in this New York Times report and study from a Wuhan hospital; however, there are currently no documented cases explicitly from airborne transmission. Exposure is a function of two elements: distance and duration. The closer and longer you are with a coronavirus patient, the more likely you are to get the disease.
Transmission through contact is the underlying principle for social distancing. It’s how Hong Kong and Vietnam were able to contain outbreaks through these non-pharmaceutical interventions.
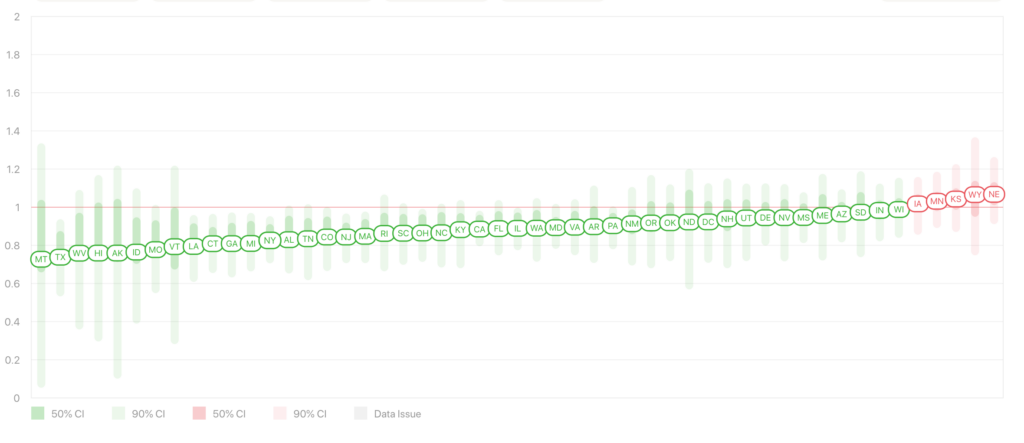
The r0, or the indicator that shows how contagious a disease is, is about 3 for Covid-19. Many studies have been done on this number. However, we must now focus on the rt, or the current transmissibility rate. As you can see from this chart, many states have succeeded in keeping this number under 1. This is critical to help slow the spread of the outbreak. Social distancing works. We cannot let it up.
This week we’ve continued to study antibody tests, which show what percentage of a population has been exposed to the disease. As the brilliant biostatistician Natalie Dean writes in the Washington Post and the New York Times, the studies show that including these asymptomatic cases make the infection fatality rate go down, but we are still a long way off from herd immunity. “There would be nothing quick or painless about reaching herd immunity without a vaccine,” she writes with Carl Bergstrom. These antibody tests in the U.S. are similar to levels in Wuhan. We are still a fair ways away from a vaccine, as this New York Times visual shows. But we can remain optimistic, as this virus seems to mutate in small ways only and remains mostly stable, according to Dr. Sanjay Gupta.
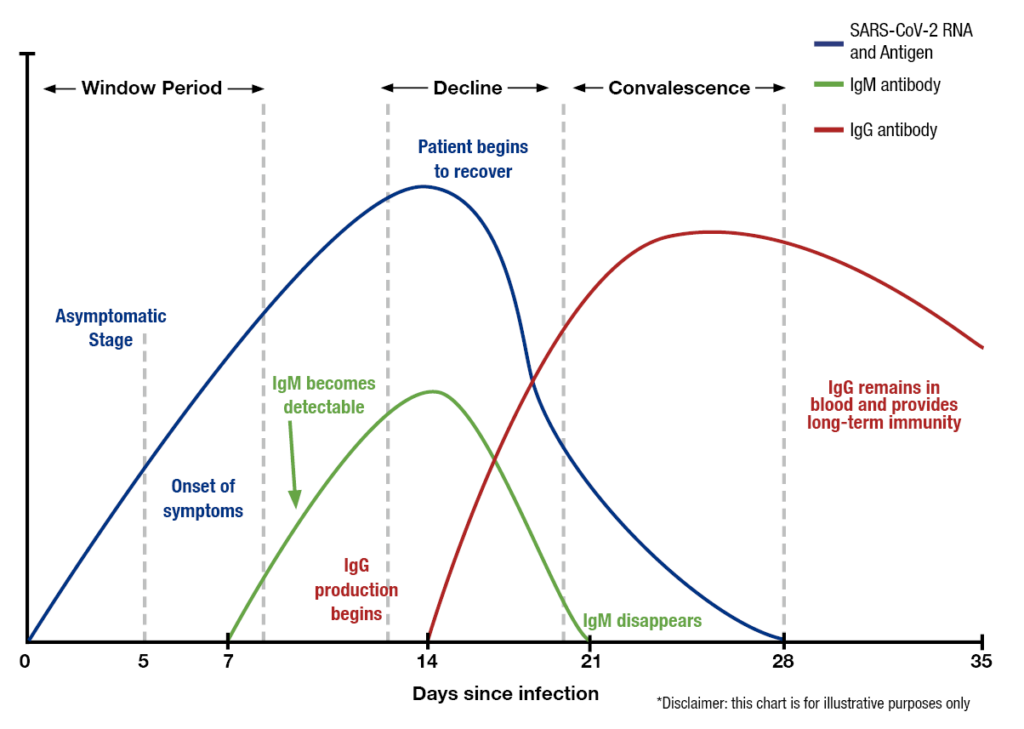
Additionally, we do not know if antibodies can provide immunity from future infection, as the WHO reports this week. However, we can continue antibody tests to gain more information and continue to improve the accuracy of these tests. These two graphics provide a great visual of how tests can detect stages of infection.
Contact tracing will be key. This week, New York announced it will hire thousands of trained contact tracers. I’d also recommend that hotels can still be used to house those patients with mild symptoms.
A big piece of news this week is the positive results from the study on the Ebola drug Remdesivir, seen here, here, here and here. Dr. Fauci first reported on this study of over 1,000 patients, which was a randomized, controlled trial with placebo. The mortality rate of patients on a placebo was 11%, compared to 8% on the drug. This is not statistically significant. However, the recovery time of patients on the placebo was 15 days, compared to 11 days on Remdesivir. This is significant. Remember this is a drug administered intravenously to people in the hospital with severe symptoms. A few unanswered questions: Which types of patients did better (based on severity of symptoms, male/female, age)? Who recovered faster? Did timing of administering the drug help — is earlier better? Does this drug decrease virus shedding/transmission?
Remdesivir is not a cure. It’s not a preventative medicine. You can’t just pop a few pills and expect your symptoms to improve. Still, experts are cautiously optimistic that this drug could work in the sickest patients.
A note on the lab theory from China. It’s unlikely, as seen here, here and here. The Office of the Director of National Intelligence “concurs with the wide scientific consensus that the Covid-19 virus was not manmade or genetically modified.”
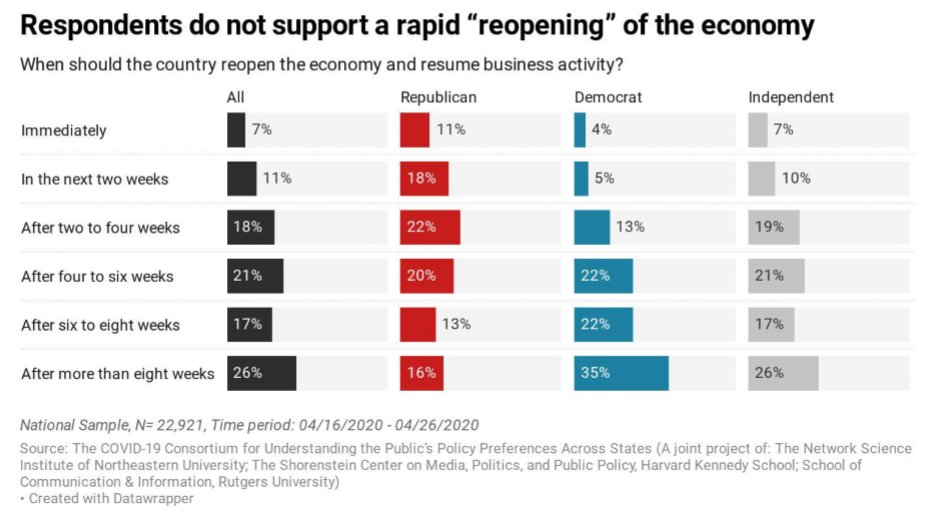
When it comes to lifting restrictions, there is a cognitive dissonance within Democrats and Republicans as seen in this insightful study.
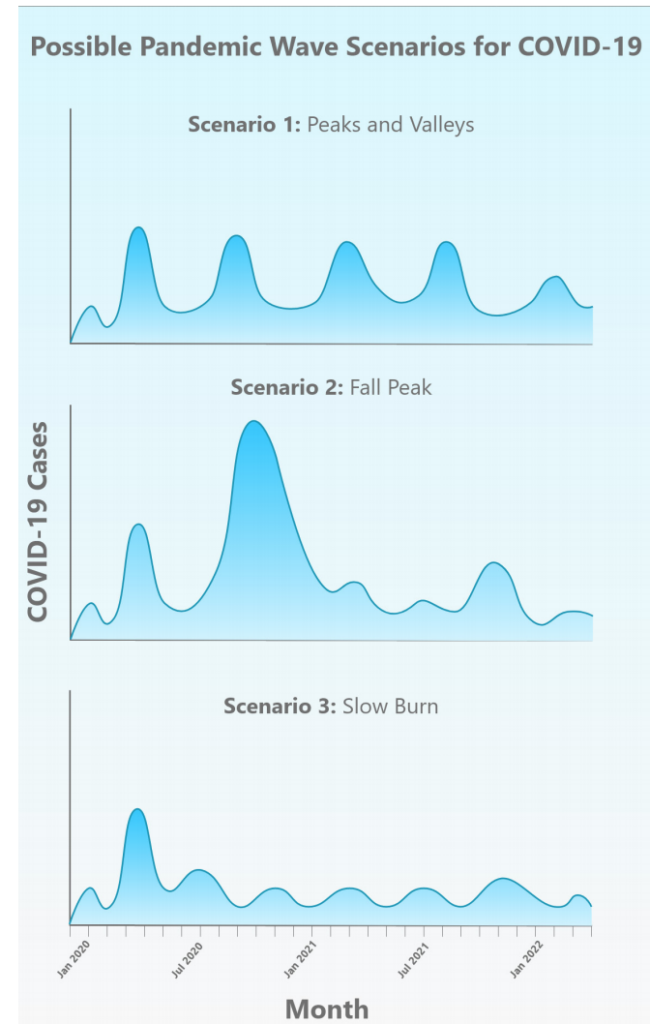
The summer will be a critical period in the fight against Covid-19, as a new study shows possible waves for the fall and beyond, predicting that the pandemic could last up to two years. Which brings us to higher education.
Higher education
Colleges have begun to announce plans for what they envision a fall semester to be like. The Chronicle of Higher Education has kept track of colleges’ plans in this table — I will be conducting further analysis of this table in the future. I think we’ll begin to see publicly, colleges announcing their commitment to holding classes in the fall — a delayed start to the spring seems unlikely among many. The higher education community was rocked when Brown University president Christina Paxon wrote in an op-ed in the New York Times: “The reopening of college and university campuses in the fall should be a national priority. Institutions should develop public health plans now that build on three basic elements of controlling the spread of infection: test, trace and separate.” She says that mass testing is an “absolute prerequisite.” I agree, but I currently question the ability for colleges to provide the ability to test their communities when the sickest patients still do not have enough tests. Ideally, testing should be a whack-a-mole scenario when colleges return. Test, isolate, treat. We should get to a point in epidemic control that a positive coronavirus case would be like controlling a campfire, not a forest fire. So much can happen between now and August, so I remain optimistic that this could be the case.
Many schools believe they will open on time, in accordance with public health regulations. Disease spreads quickly on a college campus, as seen from this norovirus outbreak. A few considerations for what this could look like:
- Colleges could consider purchasing off-campus housing to spread out students. In rural schools this is less plausible.
- Colleges could consider offering a hybrid model of online classes (large lectures) and in-person classes.
- Students want to return to campus in the fall. According to a survey in the Bowdoin Orient, 70% of non-senior students said they will not enroll in a remote fall semester. The show must go on.
- Newly admitted students are unsure as ever to commit. Colleges must increase communication outreach over the summer, especially if orientation cannot go on as planned.
- Face masks could be required.
- Shortened or adjusted academic calendars could be considered. What would a peak in, say, November, mean? We can’t just switch to remote learning — March has told us this is very difficult.
- Student input should be considered,
- Sports are a whole different issue.
- Smaller class sizes are possible.
- The most vulnerable students and faculty may not be able to attend in-person classes. Colleges should continue to bolster their remote learning technologies to deliver content to a handful of students in the event they cannot be there.
- International students may be unable to come to campus.
- Enrollment could be down, if students feel uncomfortable traveling to school from their homes far away.
- Colleges must be mindful of not overwhelming the local healthcare system in the case of an outbreak.
- Some schools may even choose those who could go back on campus. For many liberal arts schools, how do you prioritize students?
- In one of the more out-of-the-box ideas, Chinese law professor Carl Minzner suggests a “pod model,” where students would live and take classes within the same pods. This way, if there is an infection, you could force only one pod to move to remote learning. At schools with programs such as honors colleges, this could be possible. But at the vast majority of schools, the course catalog is so diverse that this would be implausible.
So there you have it. There’s a range of scenarios that colleges could be considering. I’d urge colleges at this point not to commit to anything, as the pandemic track could change over the course between now and the fall. However, during the month of June, I believe we will see a lot of decisions being made. I’ll do my best to keep reporting on these.
So do I remain optimistic about an on-campus semester in the fall? Yes. However, for the reasons stated above, college campuses could look noticeably different. We’ll continue to monitor the situation.
Study abroad and international travel
The coronavirus is a global problem (except for Antarctica, but very few, if any, study abroad programs run there). As Americans currently abroad wrestle with the decision to stay in their host country or return to the U.S., program providers such as CIEE and IFSA have begun to cancel programs. Check out this list from the Forum on Education Abroad tracking cancellations. Argentina, for example, has banned all flights to, from and within the country until September 1. Since many programs in Argentina start mid-July, adjustments will need to be made in a best-case scenario. I hold my case that the chance of study abroad programs running in the fall seems unlikely.
There was a great article in Inside Higher Ed this week about the effects of the pandemic on the study abroad industry. The effects will certainly be felt long-term. Anthony C. Ogden, the associate vice provost for global engagement at the University of Wyoming, said:
“We’ve been doing virtual internships already, we’ve been doing virtual exchanges, but one of the problems, I think, and the reason why we haven’t moved more swiftly is education abroad folks have still heavily relied on destination travel, and I have been saying for 15 years now we need to move away from that way of thinking, from ‘where’ to ‘what.”
I still don’t buy this “virtual study abroad” argument. At least half of a student’s abroad experience are the opportunities provided while in the host country. However, I’d encourage programs to come up with ways of place-based education that can be delivered virtually to continue their success.
The Good Stuff
Like last week, I’ve included this section with my favorite pieces from the week. Some are serious, and some are just plain funny.
- This CNN Town Hall with Sesame Street was the best television ever.
- This piece on the pilots who fly through the night skies to deliver coronavirus tests to the lab was inspiring. Hats off to them.
- This mini-documentary on the delivery drivers on the frontlines in New York City.
- This lip dub to “I Will Survive” of the Middlebury College international students who are still quarantined on campus.
- This amazing piece by my journalism colleague Annabelle Williams at the University of Pennsylvania on Penn nurses on the frontlines. Congrats on a great tenure at 34ST magazine, Annabelle!
Conclusion
Each week, the U.S continues to make progress in fighting the pandemic. We can’t let up now. Hang in there. This isn’t easy, I know. We look at it on a day-by-day basis.
Thanks for reading this long stream of consciousness summarizing what I’ve read, watched and reported on this week (it was a lot, as usual). I’d like to thank all the student journalists with whom I have the pleasure of working. You are all truly an inspiration and it is a pleasure to read your work. I try to include as much of your college coverage as I can in these reports. I’d also like to send my best to the Class of 2024 (college-bound seniors) on National College Decision Day. While this year brings many uncertainties for our college-bound seniors in terms of college choice, access and affordability, I appreciate you making the leap of faith and choosing the college that is right for you.
My heart goes to all who are affected by the pandemic. We have lost over 65,000 Americans and each one of them has a story to tell.
Let’s all keep doing what we’re doing and we’ll get through this together. My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments.
For more instant updates, follow me on Twitter @bhrenton.



1 Comment
Where We Stand with Covid-19 — May 8 - Off the Silk Road · May 9, 2020 at 8:46 pm
[…] possible ways going forward. You can read the first report here, the second one here and the third here. Like last week, we’ll be focusing on three major topics: a national view, higher education and […]
Comments are closed.