Welcome back to Week 43 in my weekly reports analyzing the Covid-19 pandemic and its effects on the country and higher education in a new Biden-Harris administration. For those of you reading this on my blog, Off the Silk Road, I have also launched a newsletter, where these reports can be sent directly to your email each week. Click here to subscribe.
Last week, we showed why rapid vaccination is key to saving lives and preventing future mutations. This week, we will summarize the most recent vaccine news from around the world as the mass vaccination effort ramps up in the United States.
A national look
In the Broadway musical “Hamilton,” Alexander Hamilton sings “In the eye of a hurricane, there is quiet.” In many ways, this reflects the situation our nation currently faces with the Covid-19 pandemic. Recently, we have been seeing a decline in cases and hospitalizations, and a decline in deaths will subsequently follow. However, variants mean an uncertain path ahead.
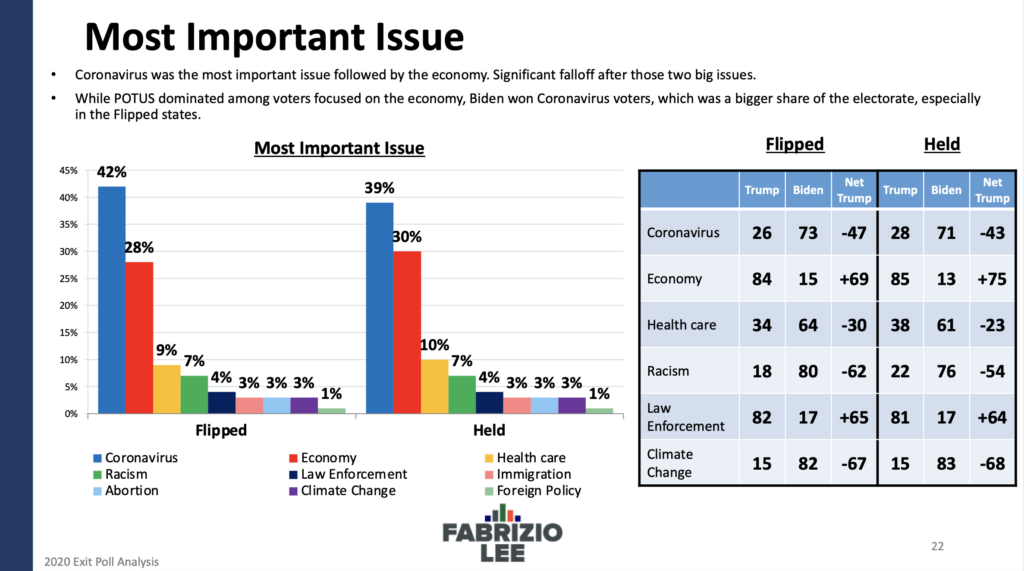
While the news cycle continues and next week will most likely focus on the former president’s impeachment trial, the virus is still with us at high levels of community transmission. According to a recent Axios-Ipsos poll, 65% of Americans do not expect to get back to something like their normal, pre-Covid life for at least six months (around late summer), with almost a third believing it will not happen until next year. Post-mortem polling from the Trump campaign’s inner pollster showed the former president’s handling of the pandemic was one of the primary reasons for his loss. This all comes as the CDC is projecting 534,000 deaths by Feb 27 and this weekend marks one year since the first known U.S. death from Covid-19.
Tonight is the Super Bowl, and we are concerned about potential superspreading effects from watch parties nationwide. “The NFL could also support and promote lower-risk alternatives, like virtual watch parties,” professors Dr. Zachary Binney and Dr. Kathleen Bachynski write in STAT. “There’s a moral imperative for the host of a major sports event to include proactive efforts to protect the community.” The CDC has released its own guidelines for Super Bowl gatherings there. On the players’ side, there is much to learn from the NFL’s coronavirus protocols, which has kept players safe and led to the Seattle Seahawks having zero cases for the entire season.
Much of the concern in discussions this week continues to revolve around variants. The CDC has confirmed 611 cases of the B.1.1.7 variant (which originated in the UK) in the U.S. The map below shows the evolution of the variant in 33 states. It is likely that it is present in more states as well; we still lack adequate genomic surveillance. Spread of the variants will possibly lead to a spike in cases in 6-10 weeks. It is up to all of us to control community transmission and prevent this from happening.
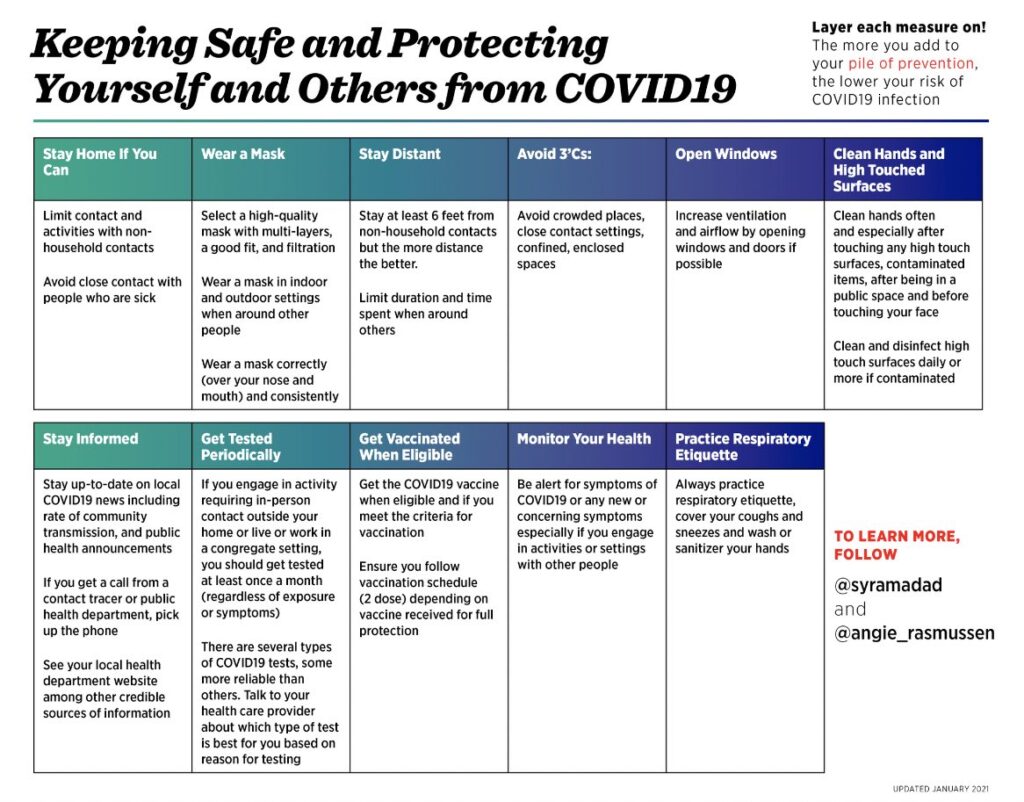
The White House is continuing to take decisive action to control the pandemic, including signing deals with six companies to produce millions of at-home rapid tests, using military personnel for vaccinations and invoking the Defense Production Act for key parts relating to the Pfizer vaccine. The CDC will release guidance on school openings next week While many of these actions will take time to realize their full potential, there are actions that we can take to minimize our risk of exposure, as seen in this table by Dr. Syra Madad and Dr. Angela Rasmussen.
Let’s take a look at some of the latest scientific developments:
- Preliminary research shows that B.1.1.7, the more transmissible variant first detected in England, has now picked up the E484K mutation as well. This mutation is the one linked to evading some immunity in South Africa and Brazil.
- A preliminary preprint from Britain shows that the B.1.1.7 variant is 35% more deadly than the standard virus.
- According to a study in The Lancet, the viral load of index cases was a leading driver of SARS-CoV-2 transmission. This emphasizes the value of reporting out PCR Ct threshold values and marked potential benefit of rapid home antigen tests.
- In Massachusetts, workers in 11 occupational groups including healthcare support and transportation and material moving had mortality rates higher than those for workers overall. Hispanic and Black workers had age‐adjusted mortality rates more than four times higher than those for White workers overall, and also had higher rates than Whites within high‐risk occupation groups.
- Researchers do not understand exactly how the disease might trigger Type 1 or Type 2 diabetes, or whether the cases are temporary or permanent. But 14% of those with severe Covid-19 developed a form of the disorder, one analysis found.
- According to a CDC report, hospital systems in states with statewide mask mandates reported a decline in weekly Covid-19-associated hospitalization growth rates by up to 5.5% after the mandate was implemented, compared with growth rates during the 4 weeks preceding implementation of the mandate.
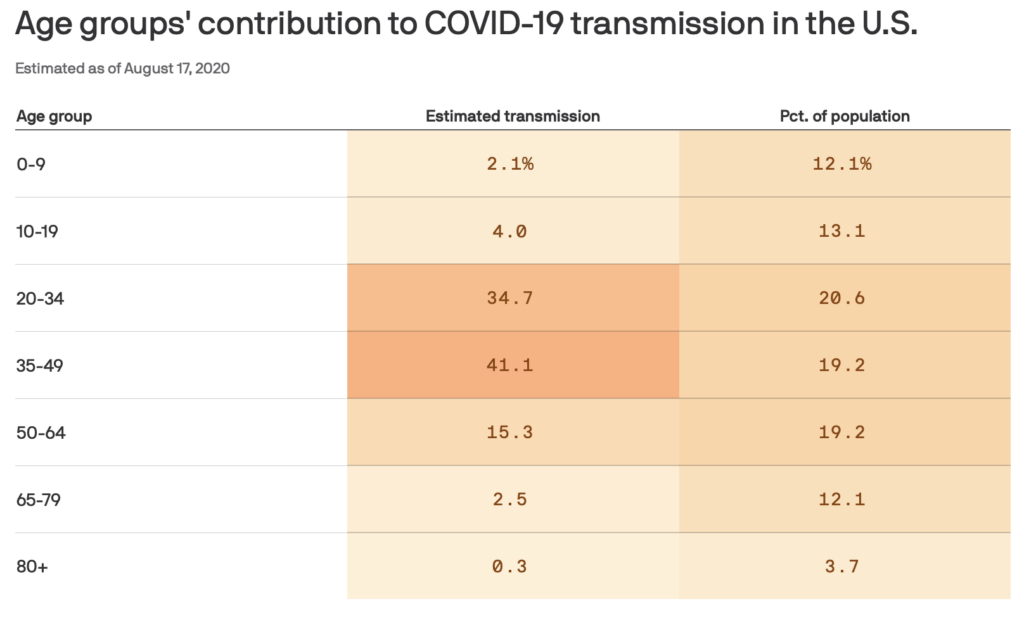
- A new study in Science estimates that individuals aged 20-49 are the only age groups sustaining resurgent SARS-CoV-2 transmission.
The U.S. hit a record for vaccinations on Saturday, with 2,218,752 doses reported as being administered between Friday and Saturday. This is promising, and we can expect the pace of vaccination to ramp up significantly in the coming weeks. However, this high number is mostly as a result of states clearing backlogs from earlier in the week. The CDC has released new data on doses administered by the day they were actually given, which you can view on my Vaccine Allocation Dashboard. The highest day so far for doses administered was around 1.7 million.
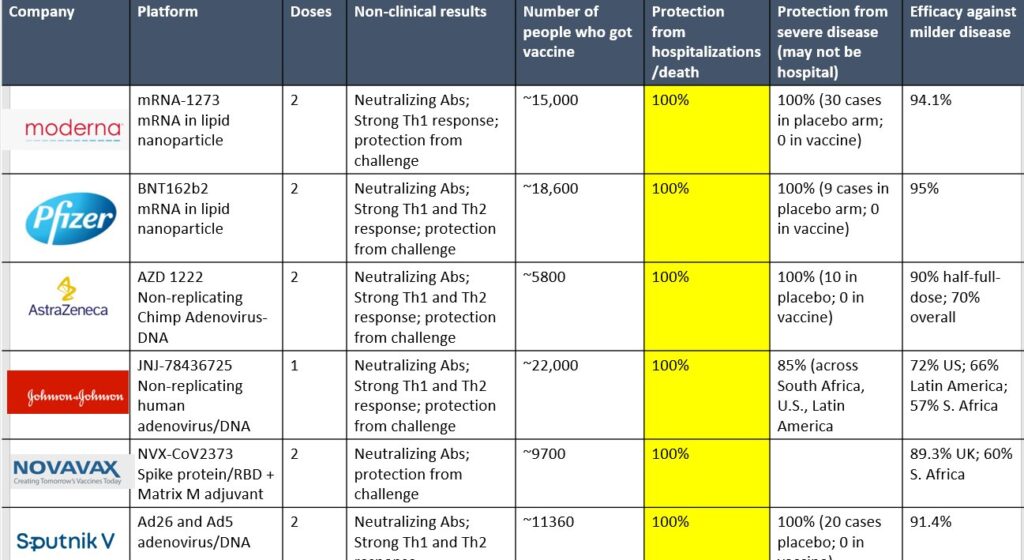
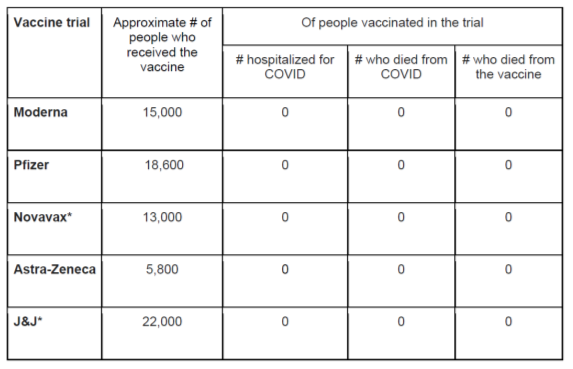
While there are currently ongoing studies (most recently in the case of AstraZeneca) showing that some of these vaccines may be less effective against certain variants, it is important to remember that of the thousands of people who received the vaccine in clinical trials, only one was hospitalized (in the Moderna trial) and none died of Covid-19 or from the vaccines. The effectiveness of these vaccines to prevent severe disease is remarkable.
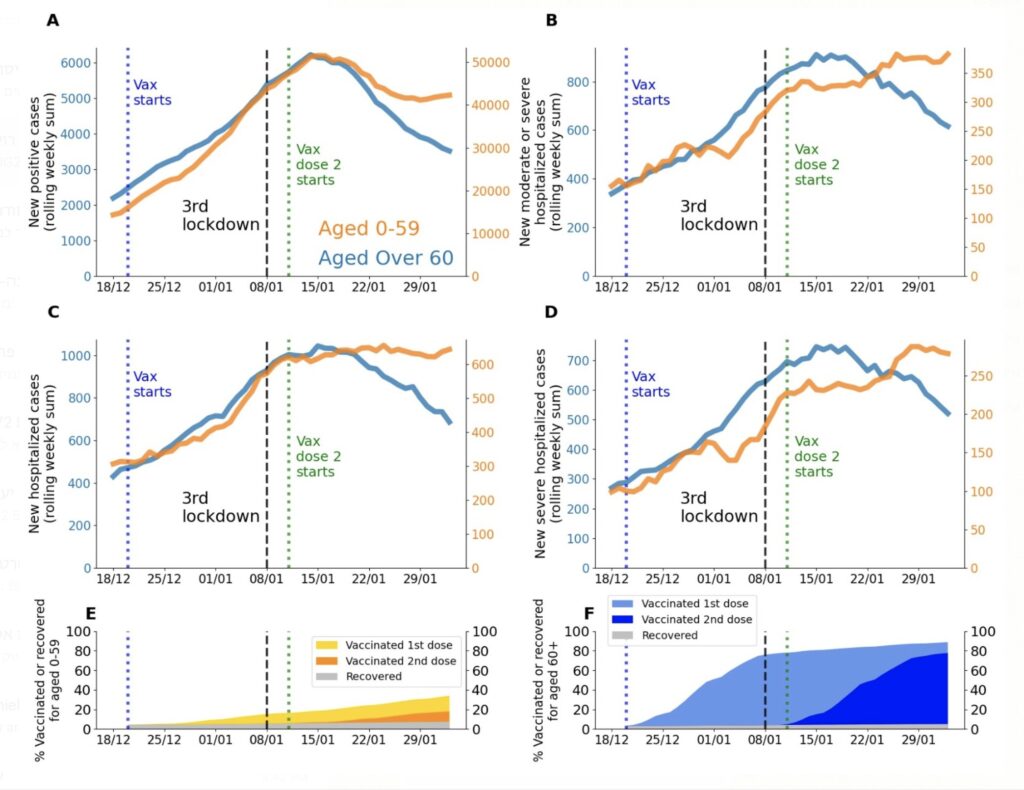
In Israel, there is preliminary data to show the effectiveness of vaccines in a large population. 77% of individuals over the age of 60 have already received both doses of the vaccine. In the past 3 weeks, among the 60+ age group, Israel has seen:
- ~41% fewer cases
- ~31% fewer hospitalizations
- ~24% less critically ill
Declines were pronounced in cities that vaccinated early on.
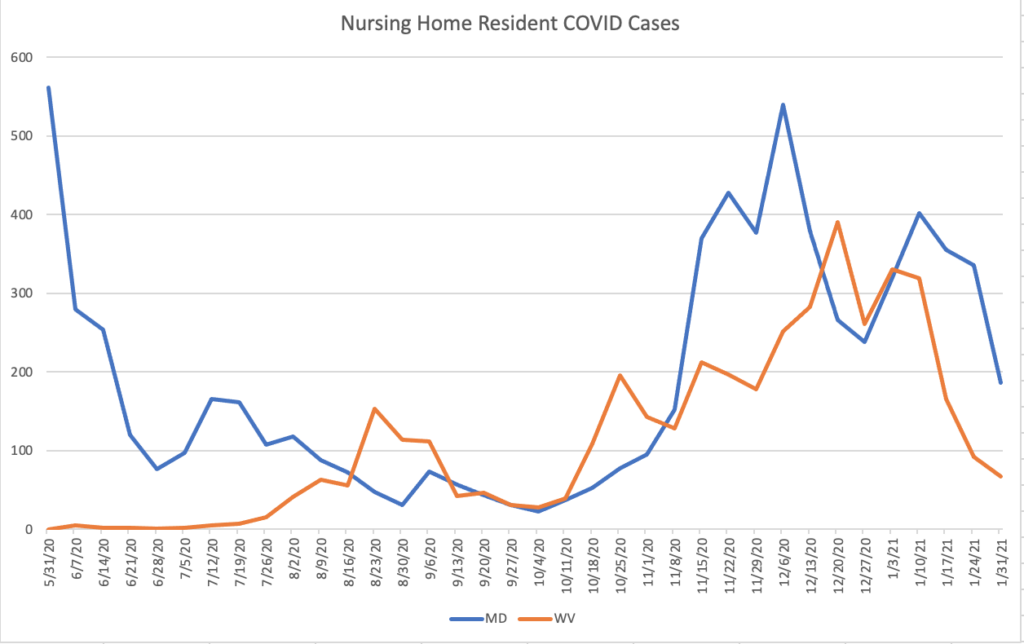
Similarly, preliminary analysis from Harvard Medical School professor Dr. David Grabowski shows that West Virginia’s early vaccination rollout in long-term care facilities likely saved lives. A drop was seen in nursing home cases two weeks after vaccinations were completed, and this decline was steeper than Maryland’s, a neighboring state with similar characteristics.
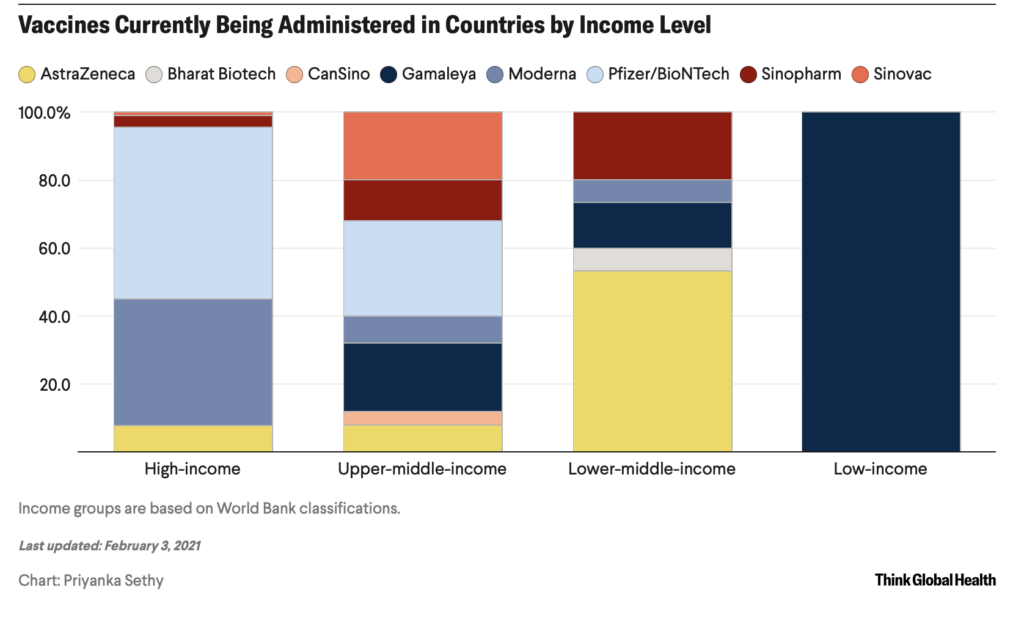
As the U.S. remains focused on its vaccine distribution, we must turn our attention to the pitfalls of “vaccine nationalism” and severe inequities found all over the world. Earlier this week, COVAX released its distribution report, showing 320 million doses allocated to 141 nations for delivery between now and the end of Q2. On average, nations can expect enough vaccine to cover 3.5% of their population (2 doses of either the AstraZeneca or Pfizer vaccine). This will not nearly be enough to ameliorate problems. An excellent analysis from Samantha Kiernan, Priyanka Sethy and Kailey Shanks at the Council on Foreign Relations shows purchase agreements for the world.
A few other updates on vaccines:
- Phase III trial results from the Russian Sputnik vaccine shows a 91.6% efficacy against symptomatic Covid-19 and 100% efficacy for severe illness. Virologist Dr. Angela Rasmussen says that these vaccines draw attention to the need for a heterologous prime-boost regimen, where we may have the potential to mix and match vaccine platforms to mount a robust immune response.
- The FDA advisory committee has scheduled a meeting on February 26 to review the Johnson & Johnson vaccine.
- According to a CDC report, during the first month of the U.S. Covid-19 vaccination program, approximately 13,000,000 people received ≥1 dose of vaccine. The demographic data show that 63% were women, 55% were aged ≥50 years and 60.4% were non-Hispanic White.
- An intriguing preprint published on MedRxiv suggests that individuals who have recovered from Covid-19 may only need one dose of the vaccine; however the logistics to implement this plan in a vaccination campaign are quite challenging.
- In addition to increasing weekly dose allocations to states, the Biden administration has announced that it will be shipping vaccine doses directly to pharmacies, with a focus on vulnerable communities. White House coronavirus response coordinator Jeff Zients told reporters that the government will ship only approximately 1 million doses per week to about 6,500 pharmacies through the new program at first. Here is a map of the states served by the top 3 pharmacy chains: CVS, Walgreens and Walmart; there will be more participating chains in the near future.
- According to a CDC report, among 11,460 skilled nursing facilities with at least one vaccination clinic conducted during the first month of the CDC Pharmacy Partnership for Long-Term Care Program, a median of 77.8% of residents and 37.5% of staff members received ≥1 vaccine dose through the program. Nursing home staff vaccination uptake is clearly an issue.
- Research from AstraZeneca’s vaccine shows a 67% reduction in positive swabs (i.e., infection) among those vaccinated. This could mean the vaccine is able to reduce transmission, but further study is needed.
- Kroger will pay its employees $100 dollars if they get vaccinated.
- The Biden administration has set up its first mass vaccination sites in California.
- Two important tools to continue to track vaccines are this chart from the Kaiser Family Foundation showing racial disparities and this dashboard from the Brown University School of Public Health and Microsoft showing vaccinations nationwide.
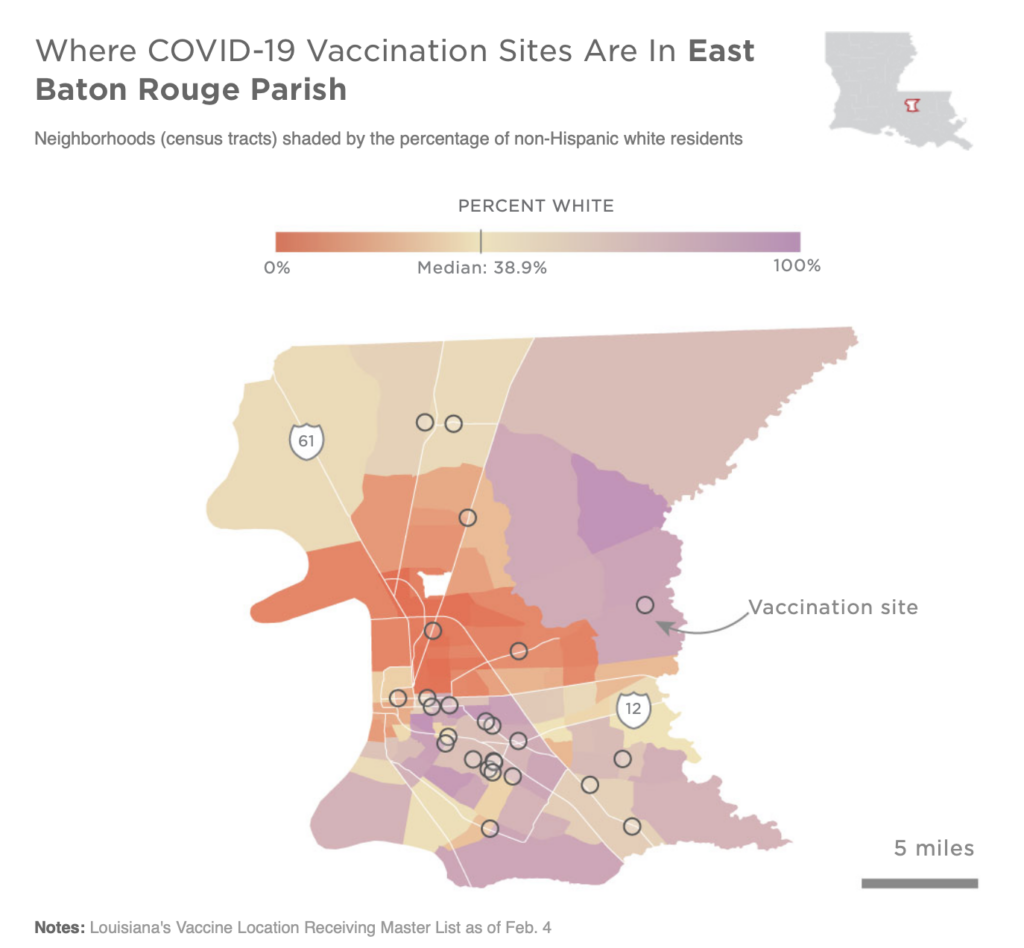
- NPR published an analysis showing how vaccine sites were lacking in many minority neighborhoods. In the coming weeks, we will continue to investigate these trends on a national scale.
Let’s move on to our discussion of higher education.
Higher education
Here’s a roundup of this week’s higher ed news:
- Davidson College’s College Crisis Initiative Director Dr. Chris Marsicano asserts that around 25% of the colleges in his team’s spring plans dataset still have “undetermined” spring plans. “There is a trend towards more in person, but the majority of changes we’re seeing are in the margins,” he told NPR. “We are not seeing many institutions go from fully online to fully in person.”
- A new working paper from the College Crisis Initiative shows county sociopolitical features had the strongest influence on colleges’ decisions to reopen with in-person instruction this fall, followed by pandemic severity and state sociopolitical features. Public four-year colleges were most strongly influenced by state socioeconomic features, and private colleges more seriously considered pandemic severity in their decision-making than public institutions.
- UT-Austin becomes the third university (after the University of Michigan and the University of California-Berkeley) to report a case of the B.1.1.7 variant in the college community.
- Boston University mourns the loss of two custodians who died from Covid-19 in January.
- “Students just aren’t feeling autonomy over their bodies and over decisions for their health right now,” one student told Inside Higher Ed. “The colleges are having an experiment, and we’re all the guinea pigs.”
- A new CDC report discusses observed mask use at six university campuses this fall. All of these universities had indoor mask mandates. 86% of people observed wore masks and 90% of those wore them correctly, with the nose and chin covered.
- Reports of maskless parties have emerged at the University of Massachusetts-Amherst and the University of Miami.
- Over the coming weeks, colleges will undoubtedly turn their attention to vaccinations. Since each state’s rollout plan differs, it is difficult to predict when colleges will be able to gain access to vaccines. I look forward to presenting data to best estimate these times. At Sacramento State University, administrators believe students should start getting the vaccine in March or April. The president of Brown University believes this will be more towards the summer. It is important to remember that some students may arrive vaccinated, including undergraduates who serve as first responders. In the context of the testing procedures on campus, they should be treated the same as non-vaccinated peers.
- The Chronicle of Higher Education’s Francie Diep reports on well-intentioned but insufficient preparations at Central Methodist University in Missouri (testing every 2 weeks but not a culture of masking, for example). 1 in 4 students contracted Covid-19 over the course of the semester.
- After UNC’s men’s basketball team’s victory over Duke last night, fans stormed the local streets, causing concerns of a superspreader event.
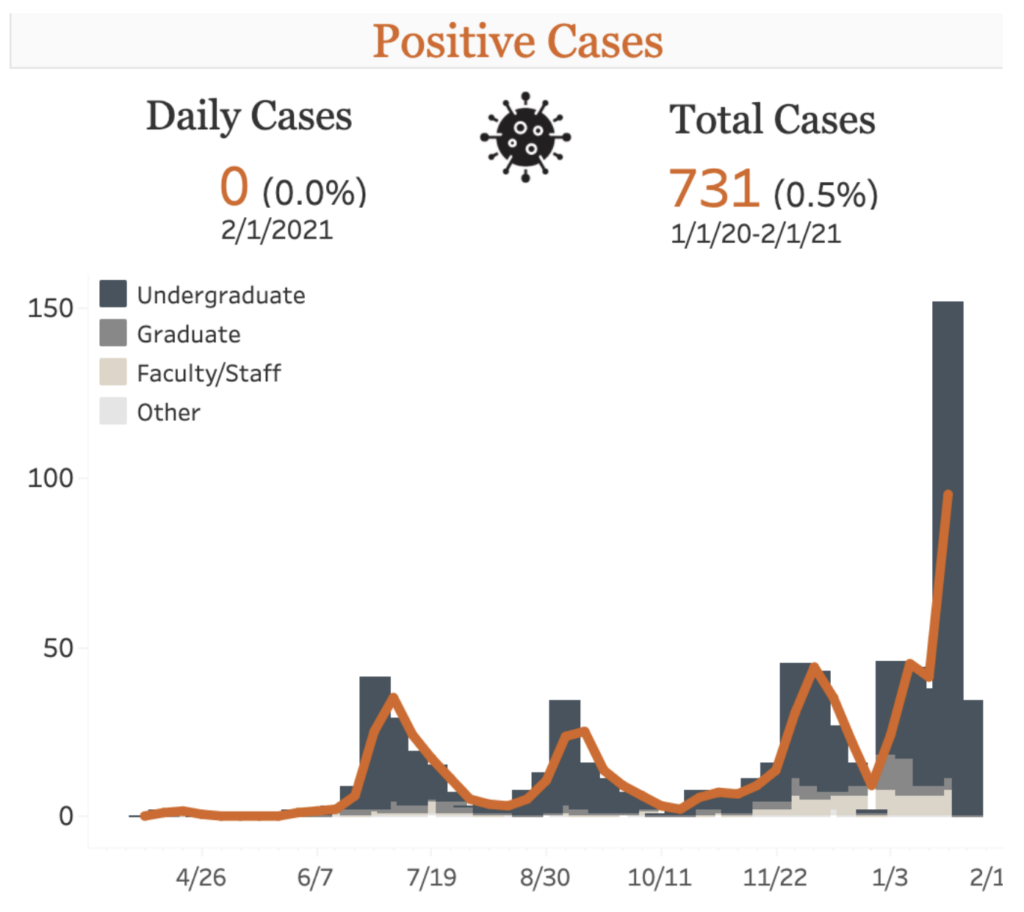
- Some colleges have seen alarming rises in their cases and test positivity rates, including the University of California-Berkeley, Duke University and Villanova University.
The Good Stuff
Let’s roll the clips of the good stuff. In my usual tradition, I feature my favorite stories from the week. Here are my Top 10.
- The New York Times takes a deep dive into the preparations for the Super Bowl halftime show.
- Days before the Super Bowl, there is a shortage of chicken wings.
- Need Super Bowl tailgate recipes for your small household? The New York Times has you covered.
- The world paid tribute to Captain Sir Tom Moore, the 100-year-old Army veteran who became a national icon through a popular fund-raiser for Britain’s healthcare system. Tragically, he passed away from Covid-19 earlier this week.
- This week we recognize the hard work of the many volunteers and employees at the COVID Tracking Project, which has been an invaluable resource for policymakers and the general public over the past 10 months. Due to upgrades in the CDC’s data system, the daily collection efforts will end in March, while analysis will continue until May.
- The National Zoo’s giant panda cubs playfully enjoyed their first snow.
- De Cecco finally reveals the reasons behind its bucatini shortage.
- Vogue Magazine profiled the new CDC director Dr. Rochelle Walensky.
- Cronkshaw Fold Farm in Lancashire, England has been offering up their goats to make spontaneous, up-close appearances in virtual meetings anywhere in the world.
- Doctors in the Academic Surgical Congress released a rendition of “Lean on Me.”
Conclusion
The United States is at a critical point in its fight against the pandemic. With cases and hospitalizations on the decline, we have between 6-10 weeks to fully ramp up vaccinations before we may see significant spread from various variants. In addition to accelerating vaccinations, we must continue to step up genomic surveillance and surge testing. The policies implemented by the Biden administration enable us to be on the offense against the virus, but it is up to all of us to ensure these actions work. We must double down on protective measures as we go into the spring.
And no, Governor Cuomo, it is still not a good time to dine indoors on Valentine’s Day. It’s exactly what the coronavirus wants us to do.
I’d like to thank all the student journalists with whom I have the pleasure of working. In the next weeks and months ahead, they will become vital in chronicling their colleges’ paths forward for the spring and beyond. Support their work by reading it.
My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments. And don’t forget to subscribe to the weekly newsletter!
For more instant updates, follow me on Twitter @bhrenton.


