Welcome back to Week 35 in my weekly reports analyzing the Covid-19 pandemic and its effects on the country and higher education. For those of you reading this on my blog, Off the Silk Road, I have also launched a newsletter, where these reports can be sent directly to your email each week. Click here to subscribe.
Last week, we analyzed alarming hospitalizations as deaths approached then-record highs. This week, we will examine troubling statistics from hospitals nationwide as a vaccine is just under 24 hours away from being administered.
A national look
I would like to begin this week’s report by congratulating Dr. Rochelle Walensky, President-elect Biden’s new appointee for CDC director, and the entire new health team. Dr. Walensky’s dedication and leadership are desperately needed to confront and resolve our country’s greatest public health crisis. Dr. Walensky’s work has been frequently featured throughout this newsletter, as she has been a driving force behind advocating for frequent testing on college campuses.
This week America witnessed a split screen of the pandemic: as scientists and trial volunteers have worked for months to get the first Covid-19 vaccine approved, a record number of Americans (over 108,000) are currently hospitalized. The data lags from Thanksgiving have passed and in the coming days we will see the effects of the Thanksgiving surge. This comes as a Bloomberg analysis found that against the advice of medical experts, many Americans still traveled for the holiday, some into Covid-19 hotspots.
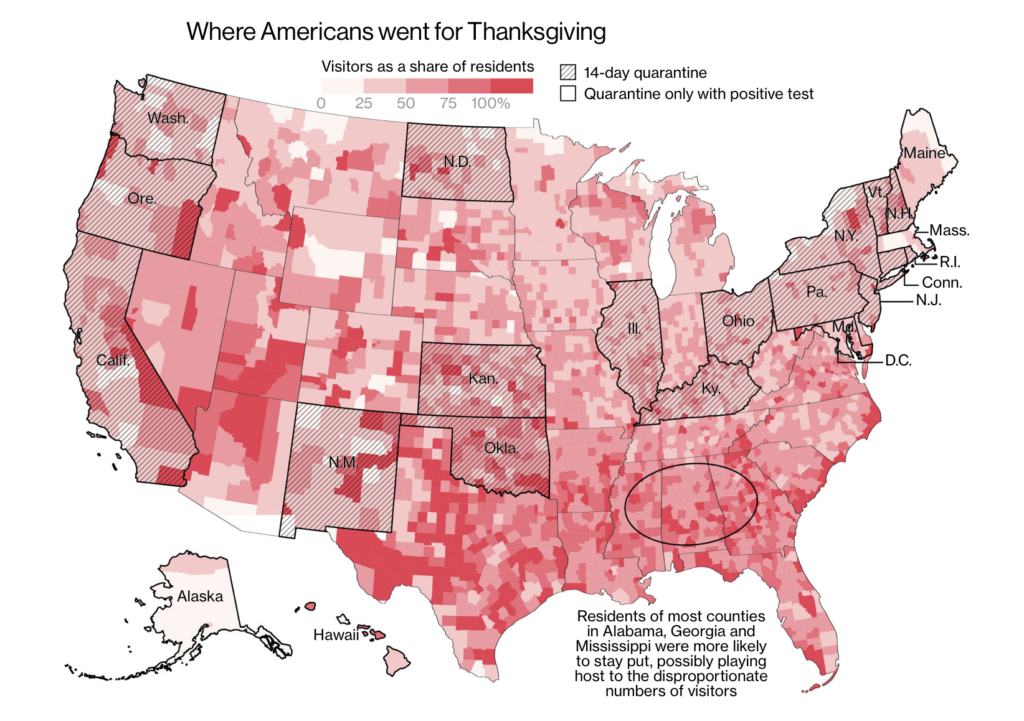
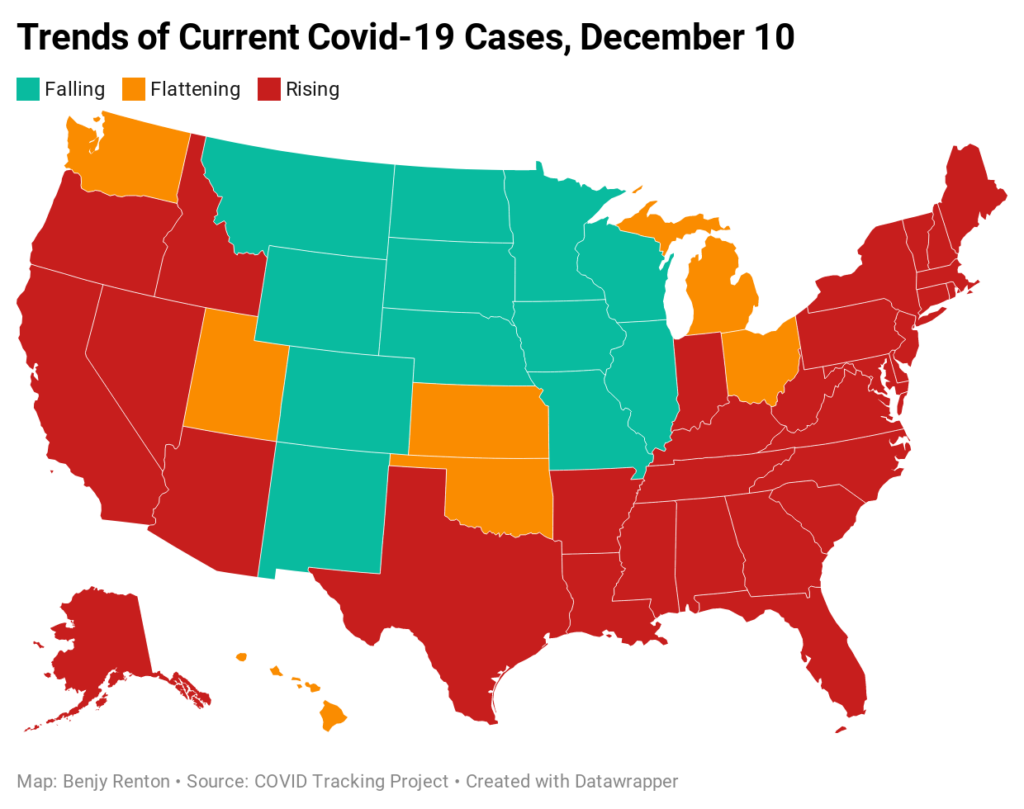
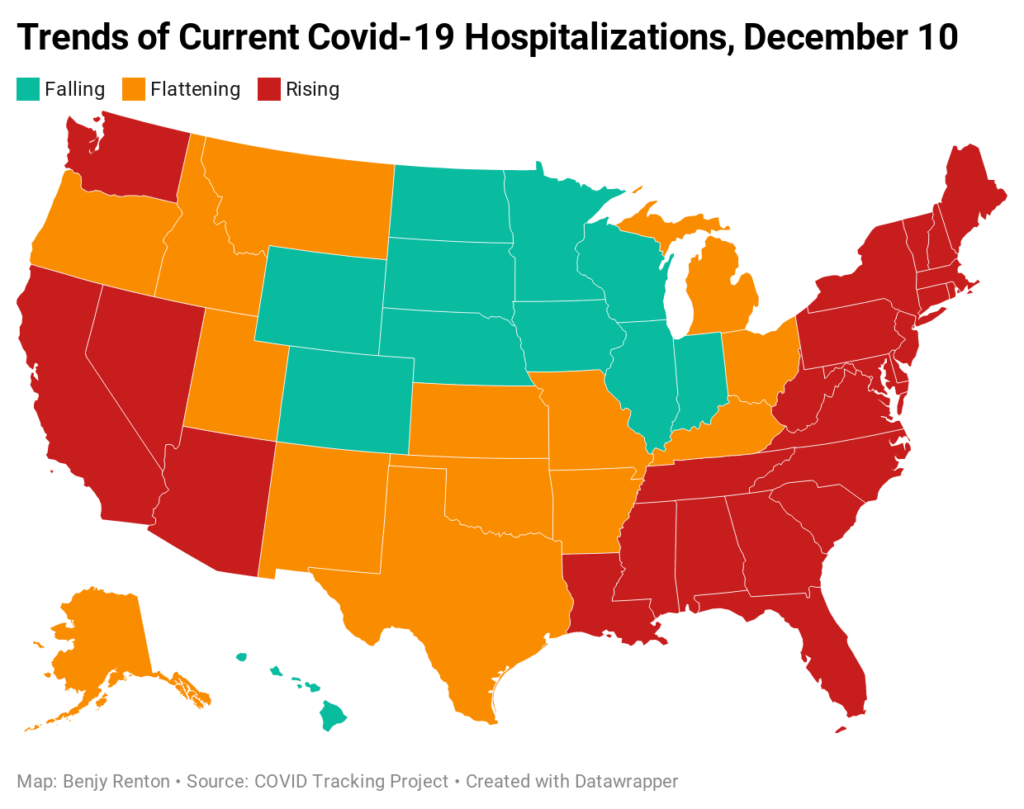
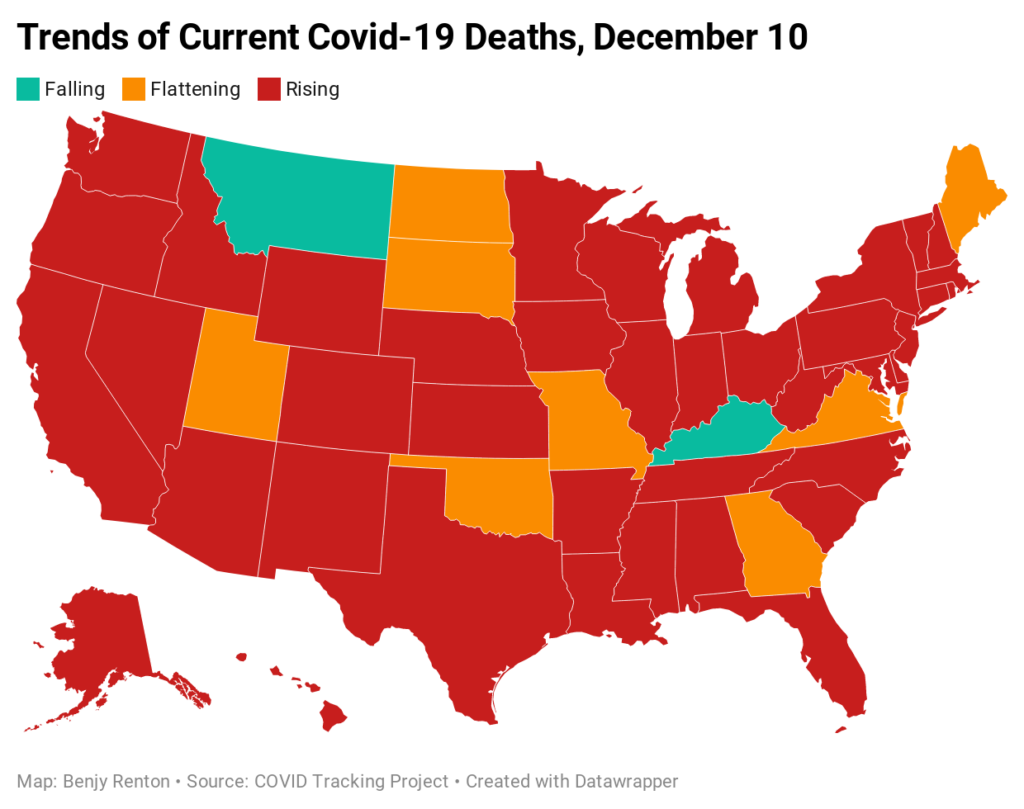
Despite the news of a vaccine, the U.S. is approaching a difficult winter. CDC Director Dr. Robert Redfield said that the daily death toll for the next 60-90 days will exceed the number of Americans who perished on 9/11. It is unfathomable to think that many Americans will die waiting in line for a lifesaving vaccine and we must do all we can do to save them. In preparation for the winter, Harvard epidemiologist Dr. Julia Marcus advocates for a public health strategy beyond simply telling people to avoid all contacts. “Our leaders have abandoned us, so of course we’re turning on each other,” she writes on Twitter. “But shaming doesn’t deter risky behavior—it just perpetuates stigma, which is counterproductive to containing the pandemic.” On Thursday, cases were rising in 32 states, flat in 7, falling in 12. Hospitalizations were rising in 26 states, flat in 14, falling in 11. Deaths were rising in 41 states, flat in 8, falling in 2.
Hospitals are severely overrun. This week, the Department of Health and Human Services released new facility-level data for hospitalizations in the U.S. It paints a grim picture: hospitals serving more than 100 million Americans reported less than 15% of intensive care beds still available as of last week, according to a New York Times analysis. Unlike surge facilities, which are erected in some hospitals to accommodate an influx in patients, ICU beds are difficult to augment due to the need for specialized equipment and staff. In the coming weeks (HHS is expected to update this dataset every week), we will continue to examine these data. Journalist Betsy Ladyzhets has mapped hospitals and capacities here.
Covid-19 continues to affect the highest echelons of the federal government, as Trump’s lead attorneys Rudy Giuliani and Jenna Ellis tested positive after attending multiple events across the country with frivolous lawsuits attempting to overturn the election. While Mayor Giuliani received special treatment in the hospital, it is important to note that most Americans are not friends of President Trump and do not get exclusive access to expensive treatment. “Covid-19, of course, doesn’t care whether you are rich, poor, Black, white, young or old,” MSNBC anchor Stephanie Ruhle writes. “The only way we can get through this is if we have a system that works for everyone, and after having Covid-19, I’m convinced that we do not.” We have continued to track the outbreak here.
This week, the FDA and CDC have issued an Emergency Use Authorization for Pfizer’s Covid-19 vaccine, just days after approvals were granted in the UK and Canada (at the time of writing the CDC director had yet to sign off on the final recommendation). This has been proven to be a highly safe and efficacious vaccine, and while it may come with some side effects (these are a sign that your immune system is working), it is clearly better than the alternative of contracting Covid-19. This is a monumental scientific achievement and we literally owe our lives to the scientists who have developed the vaccine.
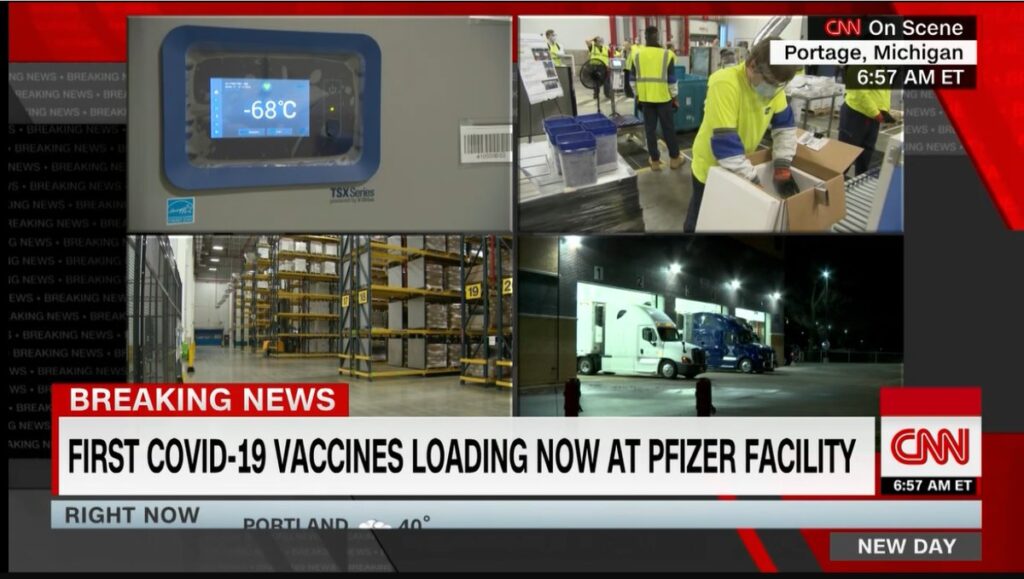
However, the end is only beginning. Most states do not have enough funding to distribute a vaccine and, with different plans, each state will prioritize different populations at different times. “The next six months will be vaccine purgatory,” The Atlantic’s Sarah Zhang writes. For the next few months, a lack of a national vaccine plan means that some groups of Americans in particular states will be vaccinated before others and the end of the pandemic will not be a simple on-off switch. To our knowledge, we do not have enough programs in place to monitor allocations, fight disinformation and increase public confidence. It certainly does not help that the White House pressured the FDA on Friday to approve the vaccine faster than its already quick timeline, nor does it help that the U.S. passed on a chance earlier in the year to procure more doses of the Pfizer vaccine. In the coming weeks, we will continue to monitor these issues as the first Americans are vaccinated. My Vaccine Allocation Dashboard here shows how many doses are allocated to each state.
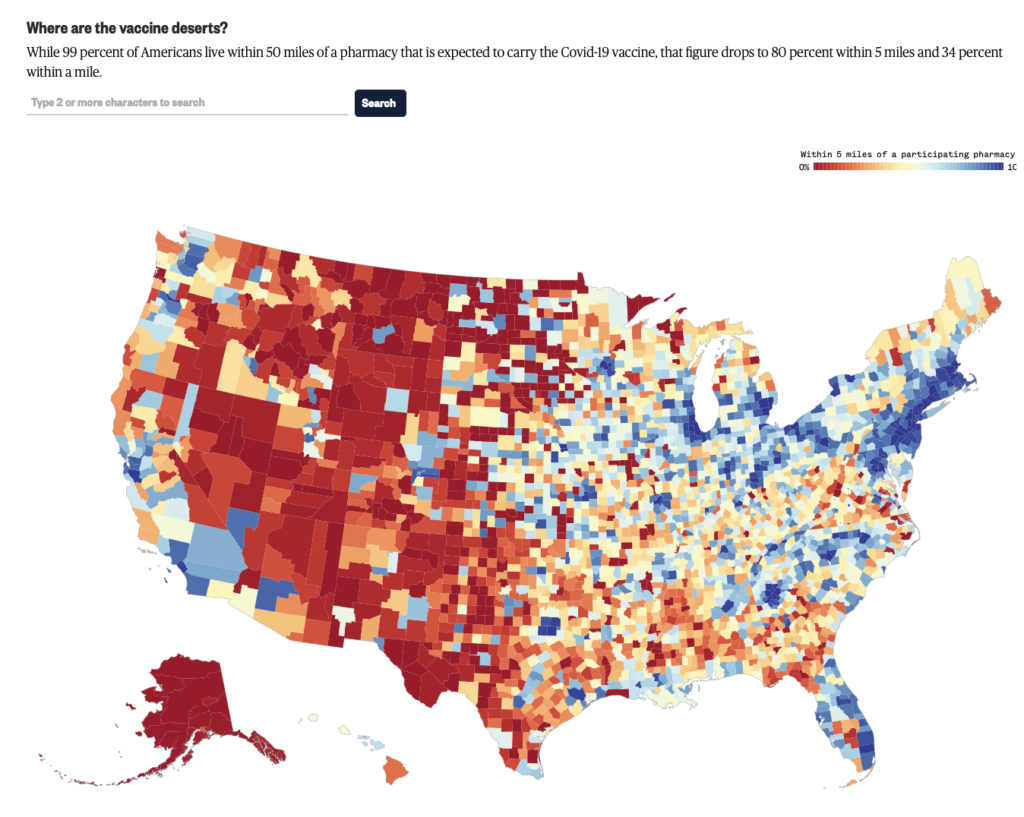
We will also continue to examine how equity and geography plays into vaccine distribution, as an NBC analysis found that 20% of Americans do not live within 5 miles of a pharmacy that is expected to administer the vaccine.
Let’s take a look at some of the latest scientific developments:
- A study using genetic sequencing published in Science found that two superspreading events in Boston in February, at a skilled nursing facility and an academic conference, led to 245,000 Covid-19 cases,
- A study published in BMJ found that healthcare workers were eight times at risk for catching Covid-19 than non-essential workers.
- A study from Switzerland of 669 people who had Covid-19 found that 32% still had one lingering symptom after 30-45 days.
- Showing the pitfalls of a “herd immunity” strategy, an area in Brazil had an attack rate of 76% with a high level of mortality, according to a study in Science.
- A preprint published on MedRxiv found that using the wrong end of the swab, or for that matter any specialized swab at all, does not impact the ability for viral detection.
- “We speculate that our respondents—and perhaps people worldwide—may be more open to the communication of uncertainty in the context of COVID-19,” according to a study using data from Germany and published in JAMA. “It may even be that admitting and communicating scientific uncertainty to the public fosters trust.”
I wanted to finish this week’s national section with a note of support and appreciation for Dr. Cleavon Gilman and Rebekah Jones. Dr. Gilman was fired from his job as an ER doctor in an Arizona hospital for speaking out and telling the truth about the severity of the disease in his state. Rebekah’s home was raided after she questioned the undercounting of Florida’s virus data earlier in the spring. When this pandemic is over, we will never forget those came forward with facts, putting their jobs and lives at risk.
Let’s move on to our discussion of higher education.
Higher education
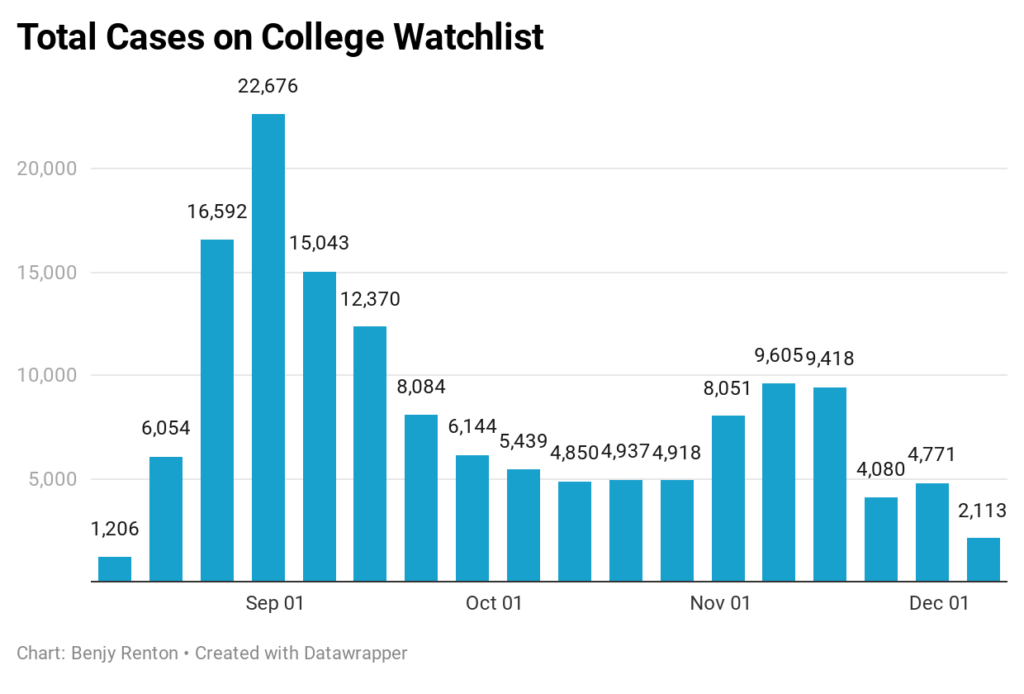
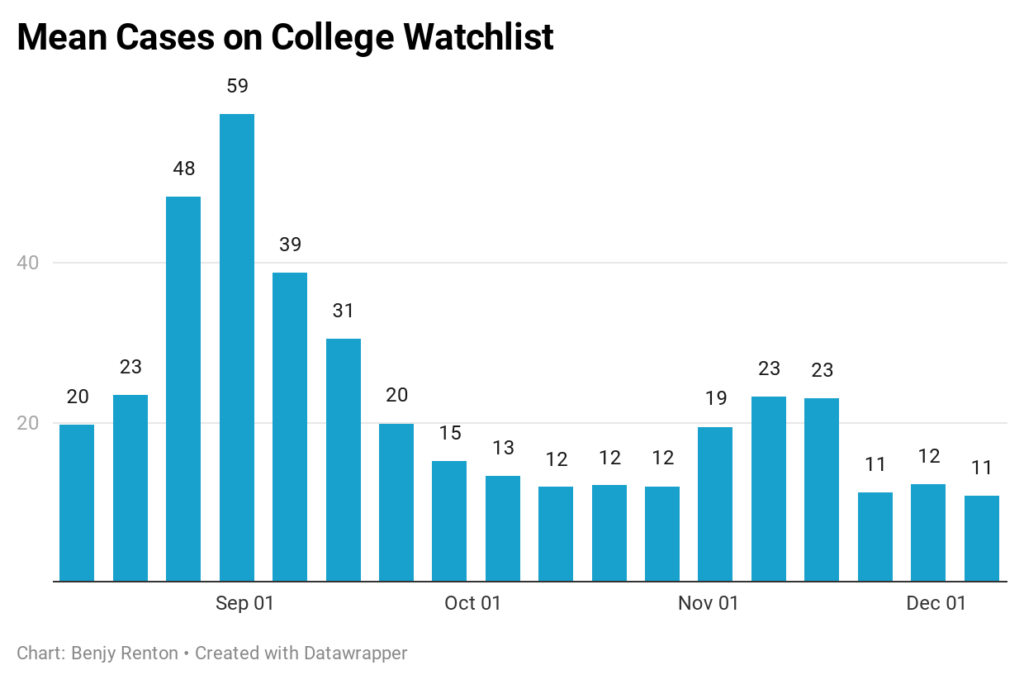
Each Friday, I update the College Watchlist, which is currently tracking 160,745 total cases at 96 colleges across the country. At the top of my list of cases in the last 7 days are:
- Brigham Young University – 236
- University of Georgia – 175
- University of Illinois – 165
- Ohio State University – 159
- Texas A&M – 112
A small number of schools have stopped reporting for the semester and many currently have no students left on campus. However, some (including Boston University) have recorded small post-Thanksgiving spikes. There were 2,113 cases recorded in the last 7 days.
Here’s a roundup of this week’s higher ed news:
- The Wall Street Journal’s Maya Goldman reports on how many colleges will use lessons learned from the fall to guide the spring.
- Due to a worsening pandemic nationally, I expect more and more colleges to push back their in-person spring start dates. Bates College is the latest to do so.
- “The most important quality of a successful contact tracer is empathy,” University of Florida contact tracer Emily Klann writes. “It is important to build trust, not only to acquire information, but also to ensure that members of the community feel acknowledged and supported.”
- “The post-pandemic campus, wherever it is, will have a renewed, more dynamic sense of place, not a diminished one,” Middlebury president Laurie Patton writes in Inside Higher Ed. “Remote learning has deepened our students’ place-based sensibility.”
- The Texas Tribune’s Kate McGee reports on two vastly different approaches to the fall semester at Texas Tech and the University of Texas-El Paso.
- This story published in The Chronicle of Higher Education about Purdue illustrates why we cannot just use cases as a metric for “success”: “Faculty, staff, and some Purdue students have a different assessment of the semester. They are tired and stressed.”
- A New York Times survey of more than 1,900 American colleges and universities has revealed more than 397,000 cases and at least 90 deaths since the pandemic began. A separate analysis found more than 6,600 college athletes, coaches and staff members have tested positive for the coronavirus this year.
- According to reporting from The Washington Post, colleges have found that viral spread seems to move from communities to the college, not the other way around.
- Student Alex Jarecki analyzed Northeastern University’s college Covid-19 dashboard and showed why plotting positive and negative tests on the same graph is misleading. It shows the immense testing capacity, not case trends.
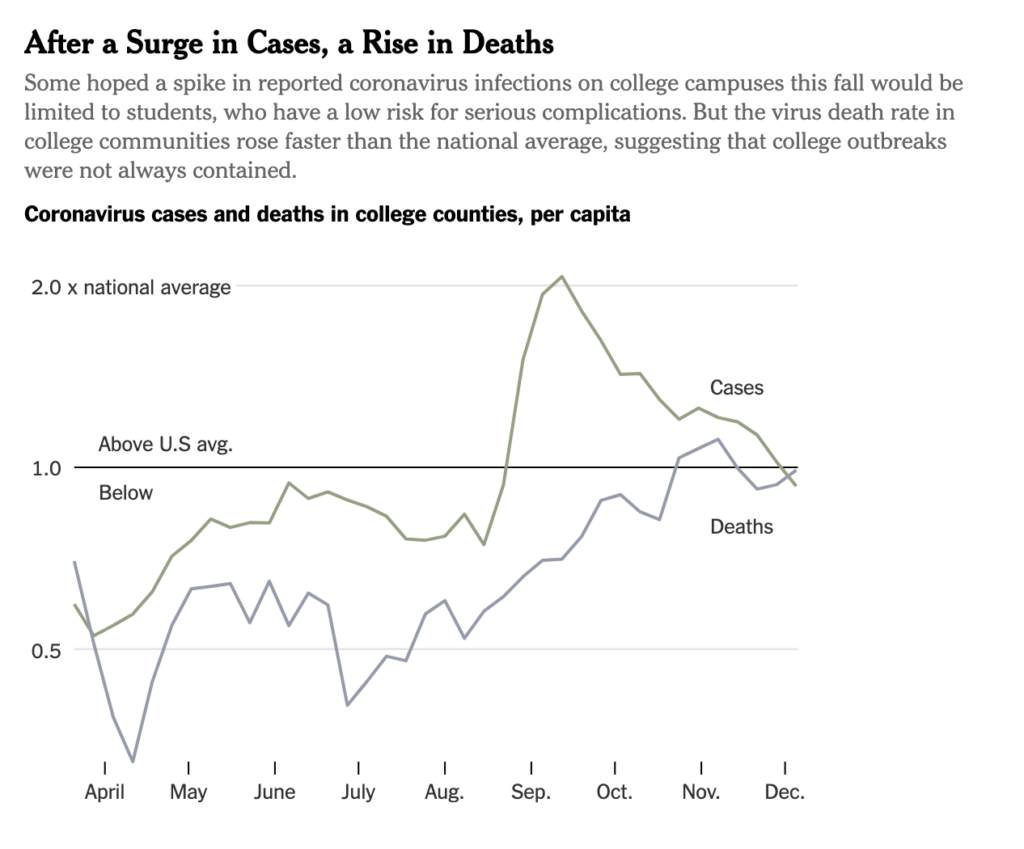
- A New York Times analysis found that coronavirus deaths in college communities have risen faster than the rest of the U.S. While without genetic sequencing it is impossible to link many college outbreaks to community deaths, it is certainly feasible that college outbreaks spread into their communities through common points in town or events off-campus. In the coming weeks we will be diving deeper into the data presented.
The Good Stuff
Let’s roll the clips of the good stuff. In my usual tradition, I feature my favorite stories from the week. Here are my Top 10.
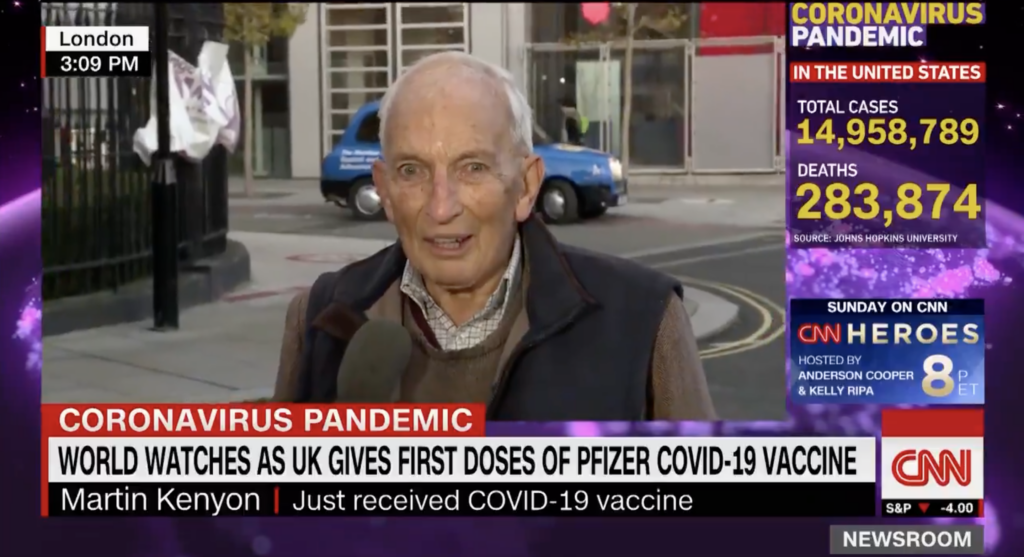
- In addition to the fact that the second person vaccinated in Britain was named William Shakespeare, 90-year-old Martin Kenyon recounted his vaccination experience on live TV. “Well, there’s no point in dying now when I’ve lived this long, is there?” he asks.
- The New York Times analyzed the bookshelves of celebrities such as Dr. Anthony Fauci and Chris Rock.
- Jimmy Fallon and Andrew Rannells performed a medley of Broadway songs as part of their newly created “2020: The Musical.”
- Students across the country have been thanking their teachers on Zoom with special group messages.
- Breakdancing has now been confirmed as an Olympic sport for 2024.
- Letters to Santa reveal the toll the pandemic is taking on kids.
- The New York Times published its 2020 in Pictures photo story.
- Vermont’s virus response has showcased the versatility of the state’s National Guard.
- Singer Chris Mann performed a parody of “12 Days of Christmas” entitled, “12 Days of Quarantine.”
- Disney and TikTok fans, rejoice! Ratatouille the TikTok Musical will come to life in January as a one-time-only benefit performance.
Conclusion
“The United States is entering a long, dark period, and the pandemic is already breaking records from the spring,” editors at the COVID Tracking Project write. Before vaccines arrive on a large enough scale to make a major impact on infections, all estimates point to the pandemic accelerating in the coming weeks. Cases in the U.S. increased from 15 to 16 million in just four days this week. More Americans will continue to die, tragically passing so close to the opportunity to be vaccinated just a few short months later. We must do all we can to save our hospitals from more strain this holiday season and perpetuate a cycle of mass deaths. We know these vaccines are safe and will prevent individuals from suffering from this disease. We just need people to live long enough to see that day.
I’d like to thank all the student journalists with whom I have the pleasure of working. In the next weeks and months ahead, they will become vital in chronicling their colleges’ paths forward for the spring and beyond. Support their work by reading it.
My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments. And don’t forget to subscribe to the weekly newsletter!
For more instant updates, follow me on Twitter @bhrenton.


