Welcome back to Week 45 in my weekly reports analyzing the Covid-19 pandemic and its effects on the country and higher education in the new Biden-Harris administration. For those of you reading this on my blog, Off the Silk Road, I have also launched a newsletter, where these reports can be sent directly to your email each week. Click here to subscribe.
Last week, we examined new concerns about variants as the CDC released new guidance on schools and vaccinations continue. This week, we will discuss the effects of severe weather across the country as the current national picture continues to improve and variants continue to spread. We will also look at some outbreaks at colleges.
A national look
First, we must take a moment to express our deepest sympathies for those affected by winter storms and deep freezes in Texas. Over 26 people have died in the state, including an 11-year-old boy. In order to build a healthier future, we need to take the time to address our relationship with the environment and ensure we build sustainable solutions to counteract the effects of climate change.
Cases, hospitalizations and deaths in the U.S. continue to drop, and while they are not yet down to summer levels, they are improving. The Atlantic’s Derek Thompson attributes these trends to four factors:
- Changes in behavior
- Seasonality
- Partial immunity
- Vaccines
It is quite likely all of these factors play a role in the national picture, but it is critical that we maintain this progress. The CDC has confirmed 1,523 cases of the B.1.1.7 variant in 42 states, which is most certainly an undercount. Researchers have reported 7 variants in multiple U.S. states, all containing the same mutation. Additionally, medical experts are concerned about possible effects of the winter storms on viral transmission. As disasters always disproportionately affect the most vulnerable, gatherings of multiple families indoors to shelter and stay warm may also harbor the virus. Testing and vaccination sites throughout the country have been closed this week due to a lack of power. However, a new survey draws attention to the U.S.’ continued lack of testing, even without a winter storm: According to a STAT poll, close to 50% of Americans surveyed who wanted a test were unable to access one due to proximity issues or long wait times. Throughout many counties in the U.S., residents live miles away from a testing site.
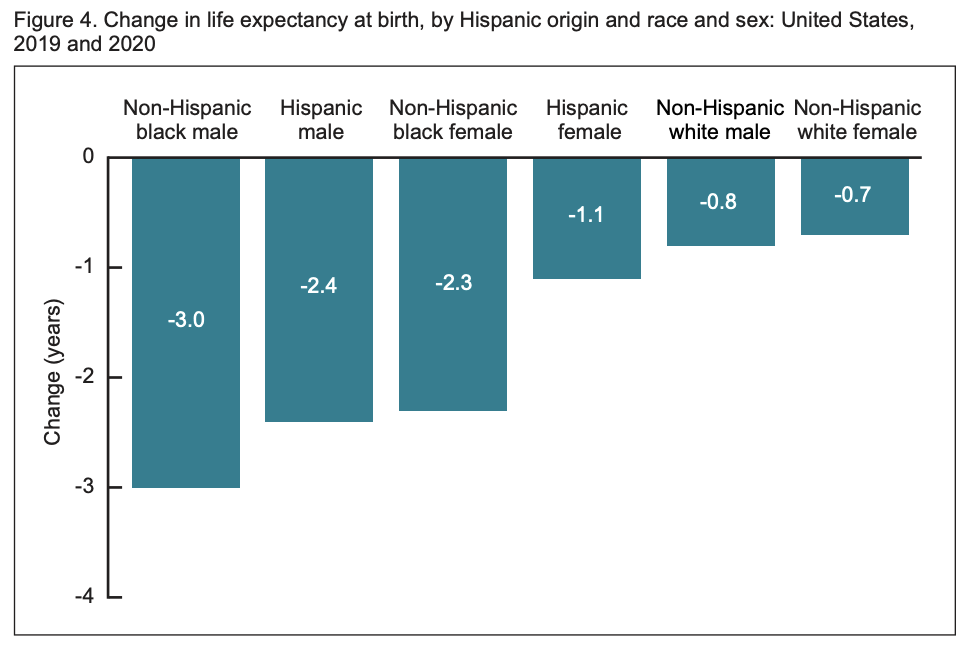
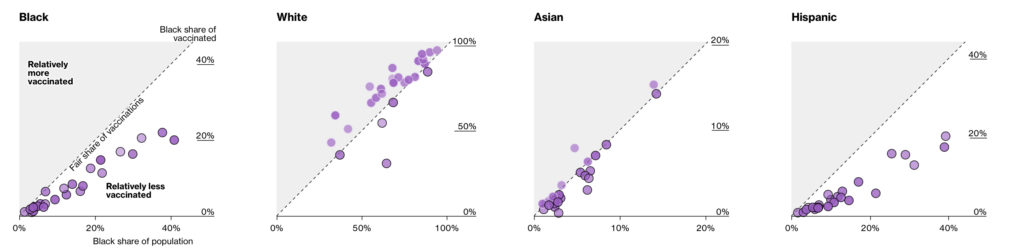
One of the more shocking statistics this week came from a new CDC study. Researchers concluded that life expectancy in the U.S. dropped a full year from 2019 to 2020, the largest drop since World War II. Like much of this pandemic, there were racial and ethnic inequities; life expectancy of the Black population declined by 2.7 years in the first half of 2020, slicing away 20 years of gains. The effects of this pandemic will be felt for years to come.
President Biden and his administration continue to take aggressive action to combat the pandemic. This week, he announced the allocation of $650 million to testing in K-8 schools and congregate settings, $815 million to testing supply manufacturing and $200 million to genomic sequencing, in addition to $4 billion to COVAX, an initiative to equitably distribute vaccines around the world. President Biden also visited the Pfizer manufacturing facility in Michigan, where he address his plan to have enough doses for 300 million Americans by the end of July.
As we continue into the spring, the variants are the greatest wildcard between now and an optimistic summer. Brown University School of Public Health Dean Dr. Ashish Jha believes that by the summer, many Americans will be able to travel and gather (unlikely in large gatherings, but among friends and family). He says that while the variants do pose concern, there is currently little reason to doubt the adequate protection of the vaccines. Until then, we must continue to protect each other and resist the temptation to ease restrictions too early. A model published in The New York Times found that if the U.S. accelerates to 3 million shots per day, “herd immunity” may be reached by May with 90,000 further deaths between now and then.
Let’s take a look at some of the latest scientific developments:
- According to a preprint from Harvard researchers, a possible explanation for the B.1.1.7 variant’s increased transmissibility is that the variant causes longer infections at peak viral load in individuals.
- An article in the American Journal of Obstetrics and Gynecology shows that among 20-39 year old adults in Washington State, the SARS-CoV-2 infection rate in pregnancy was 13.9/1,000 deliveries compared to 7.3/1,000 in 20-39 year old adults. Pregnant women are at increased risk for complications from Covid-19 and thus explains why many states are prioritizing them for vaccinations.
- New commentaries and studies from the CDC draw attention to the dangers of variants spreading in the U.S. In Zambia, the B.1.351 variant (first detected in South Africa) spread rapidly through the country. Similarly, the B.1.1.7 variant has been detected multiple times in Minnesota.
- Two new studies this week highlight the long-term effects of Covid-19. In one published in JAMA, PTSD was found in 30% of Covid-19 patients. In another cohort of individuals, 30% reported persistent symptoms more than nine months after diagnosis.
- A preprint published on MedRxiv found several factors connected to Covid-19 infection, including household crowding, visiting places of worship, indoor dining at restaurants and bars and inconsistent mask use while grocery shopping.
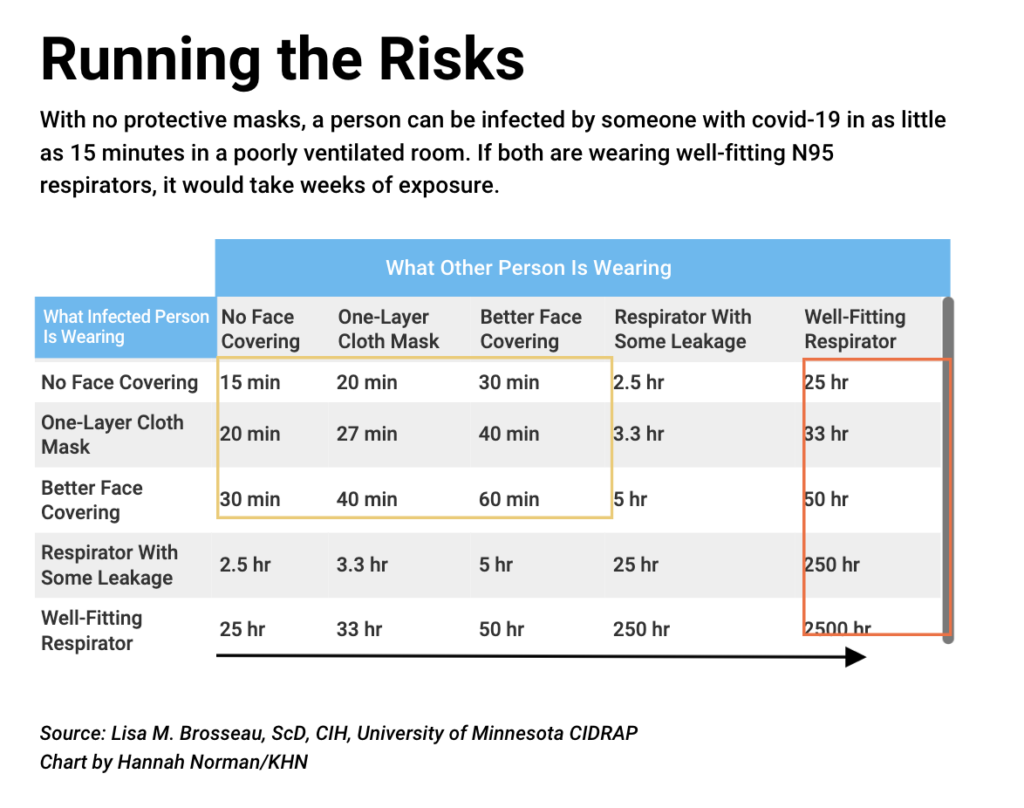
- A prominent group of academics is pressing the Biden administration to move faster and take stronger action to protect high-risk workers from airborne exposure to the coronavirus, urging enforceable standards to help safeguard risky workplaces including health care, food processing and prisons. This table shows the risk of infection in a poorly ventilated room by the type of masks individuals are wearing.
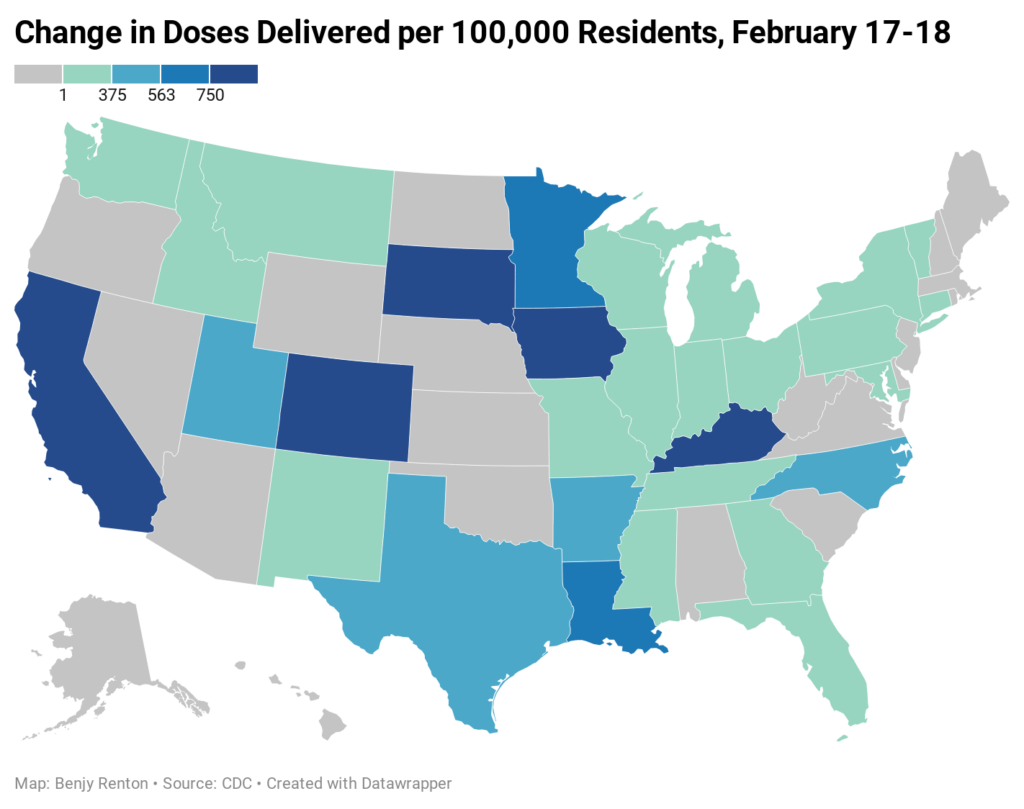
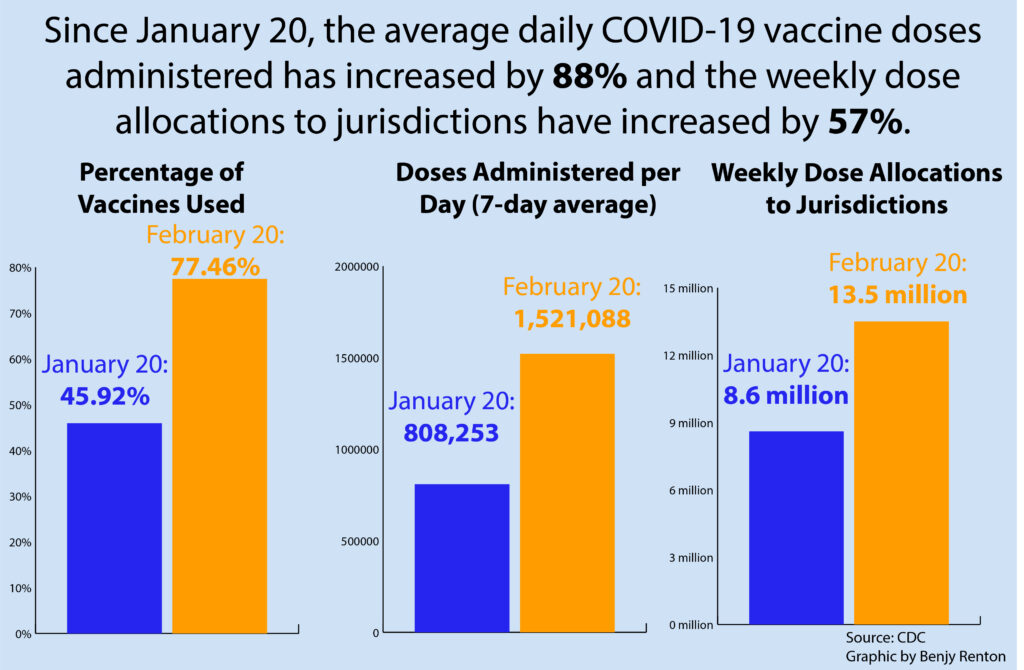
Severe winter weather throughout much of the U.S. had a sizable impact on vaccine distribution this week, shutting UPS’ Worldport hub for the first time in the company’s history. On Friday, the White House said 6 million doses were in storage and will be sent to states as soon as possible. On Thursday, 20 states reported no increase in the doses delivered in the past 24 hours. The storms have contributed to a lack of supply in many sites, forcing appointments to be cancelled and second doses to be prioritized. However, on Friday we saw the first signs of supply chain recovery, and shots in arms will soon follow. Next week, 13.5 million vaccine doses will be allocated to states, a 23% increase over this week. 2 million doses will be sent through the federal pharmacy partnership.
It has now been one month since the Biden-Harris administration has taken office, and under the new leadership the country has made significant strides in vaccine rollout. We have a long road ahead of us, including recovering from severe weather, but we have seen great progress.
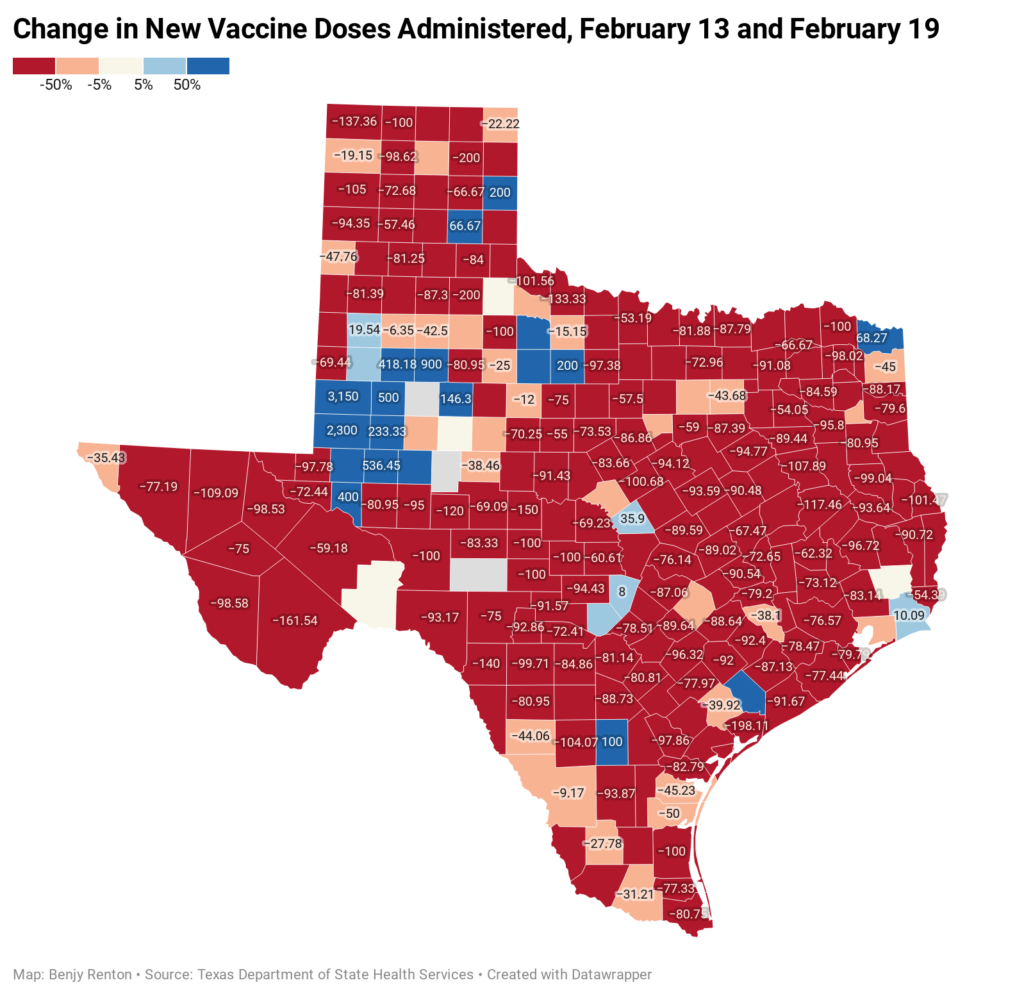
Vaccines have been severely disrupted in Texas, with many vaccination sites without power through the week. FEMA has reported more than 2,000 vaccine sites are located in areas with power outages.
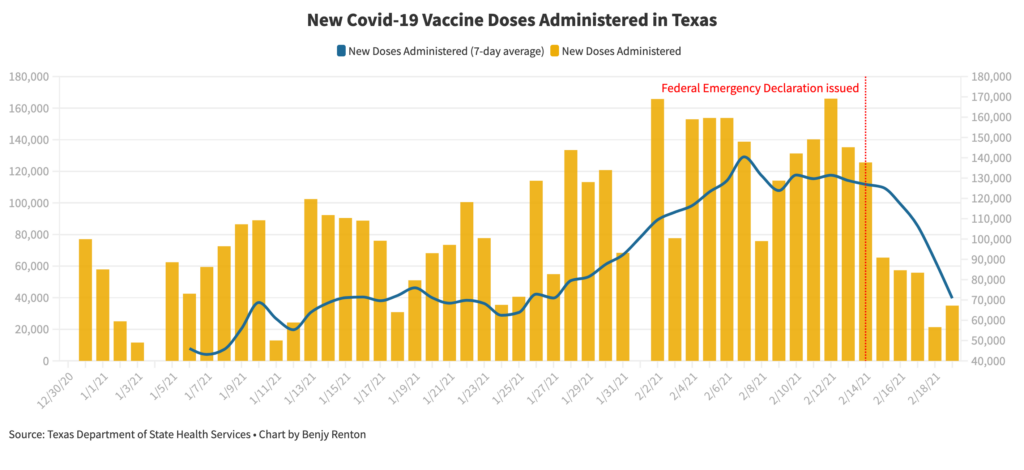
Despite these small roadblocks, vaccine production is expected to increase significantly in the coming weeks, with the possibility of the U.S. having enough capacity to administer over 3 million doses per day.
A few other updates on vaccines:
- New data from the Pfizer vaccine in Israel published in The Lancet show an 85% reduction of symptomatic Covid-19 between 15 and 28 days after patients were given the vaccine. Overall infections, including among asymptomatic patients, were reduced by 75%. Additionally, Pfizer is seeking approval from the FDA to store its vaccine at freezer temperatures from two weeks, a marked improvement from the previous deep freezing requirement.
- Another preprint study from Israel found the Pfizer vaccine to be 89.5% effective at preventing coronavirus infections, whether symptomatic or asymptomatic.
- Israel’s largest healthcare provider on Sunday reported a 94% drop in symptomatic Covid-19 infections among 600,000 people who received two doses of the Pfizer’s vaccine, in the country’s biggest study to date.
- Data published in The New England Journal of Medicine found that the Pfizer and Moderna vaccines remain effective against the B.1.351 variant (first discovered in South Africa) with reduced protection.
- Two young women in Florida dressed up as elderly “grannies” to receive their vaccines and were stopped before receiving the second dose.
- A successful vaccine campaign brings the vaccine to the people who can’t get it. In Vermont, EMS workers have been vaccinating the state’s most vulnerable. The state is also loosening quarantine requirements upon entry into the state for those who are fully vaccinated.
- Bloomberg published a useful tool to track demographic differences in those being vaccinated.
- Clinical trials have begun for pregnant women and children.”In science we’re learning about, like, genetics and stuff like that,” 14-year-old Alexandra King a vaccine clinical trial volunteer, said. “So maybe the teacher will say, ‘Oh, you really shouldn’t have to take the test, because you’re contributing to science already.’”
- According to an article in The New England Journal of Medicine, the Pfizer vaccine is estimated to have an efficacy of 92% after the first dose.
- NPR published an incredibly useful tool on how to look up eligibility and sign up for a vaccine in your state.
- After one month of reporting data, the CDC issued a report showing both Covid-19 vaccines had anaphylaxis rates of 4.5 cases per million, similar to other vaccines. No deaths were found to be related to vaccines.
- According to a preprint of a multi-state analysis in the U.S., administration of two Covid-19 vaccine doses was 88.7% effective in preventing SARS-CoV-2 infection (both symptomatic and asymptomatic) with onset at least 36 days after the first dose. Expect to see more studies published in the coming months on the efficacy of these vaccines to prevent transmission.
- A commentary published in JAMA focuses on bringing the vaccine to hardest-hit areas, including vaccinating entire hard-hit communities and partnering with civic and community leaders.
- Kaiser Family Foundation published a comparative analysis of the high-risk medical conditions states are prioritizing.
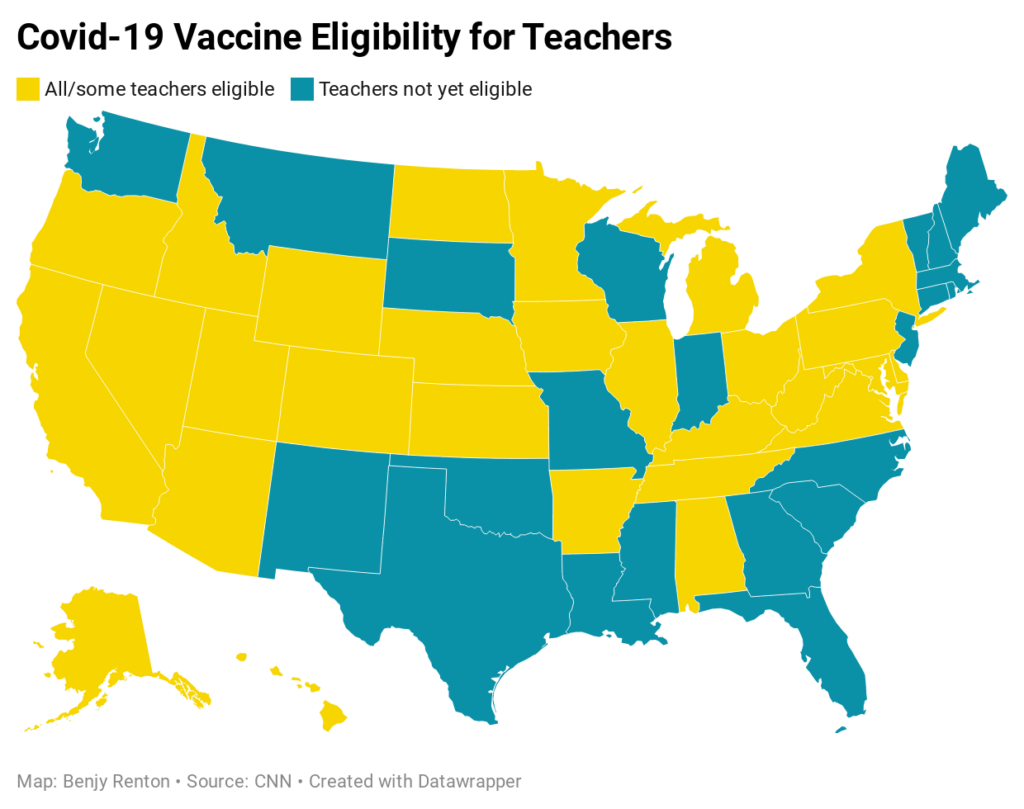
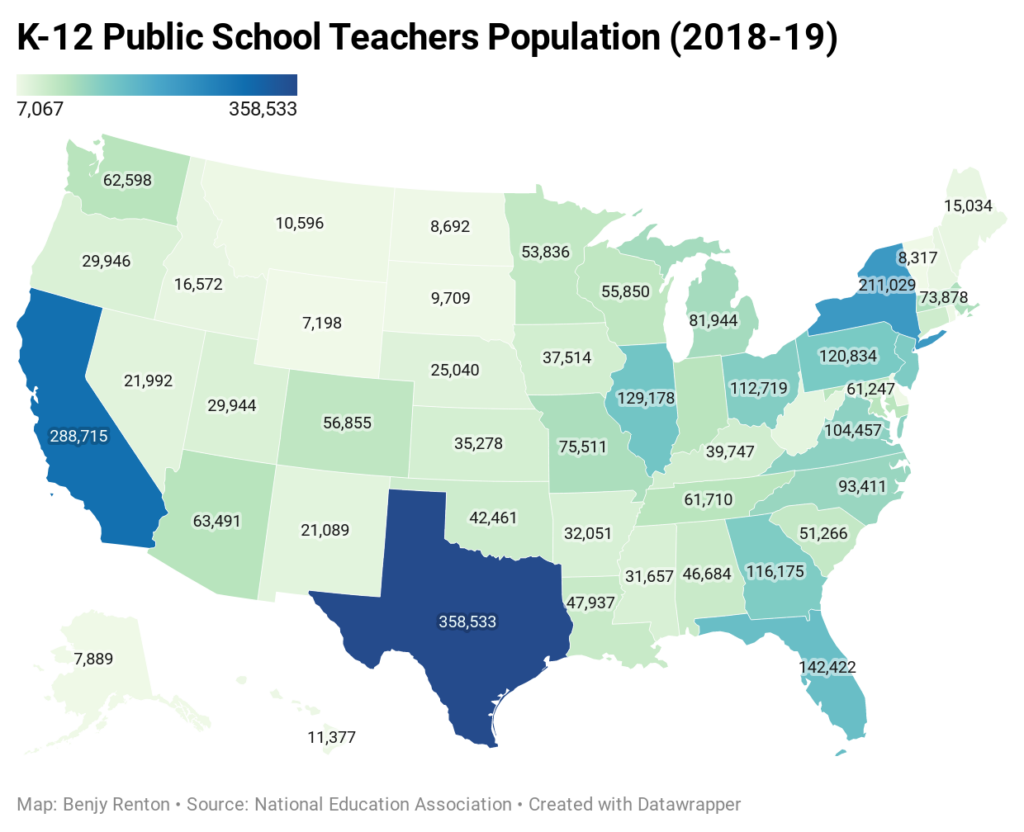
- Earlier in the week, Dr. Jonathan Reiner floated the idea of using the first batch of Johnson & Johnson vaccines to vaccinate all of America’s teachers and open schools in April. There are ~3.2 million teachers in public schools and 0.5 million in private schools — 1.1% of the U.S. population. Assuming the J&J vaccine is authorized early late February/early March, the company has promised ~12 million out of its 100 million doses to be delivered sometime in March. Taking ~¼ of that first batch would be sufficient to vaccinate all teachers in the U.S. You can read more about this plan in my analysis here.
Let’s move on to our discussion of higher education.
Higher education
Despite case counts subsiding nationally, many colleges and universities are seeing record-high case counts and multiple outbreaks, with some eclipsing fall semester case totals. Earlier in the week, I posted an analysis on Twitter with six universities currently experiencing outbreaks. From this table, we notice that colleges have been reaching case peaks ~14 days after the start of classes.
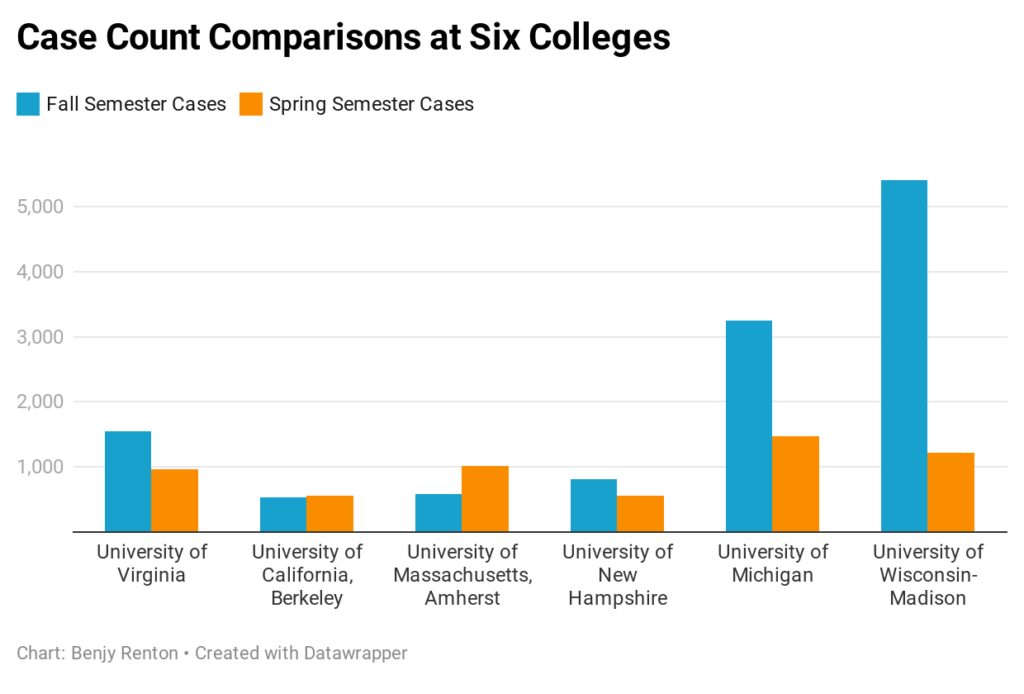
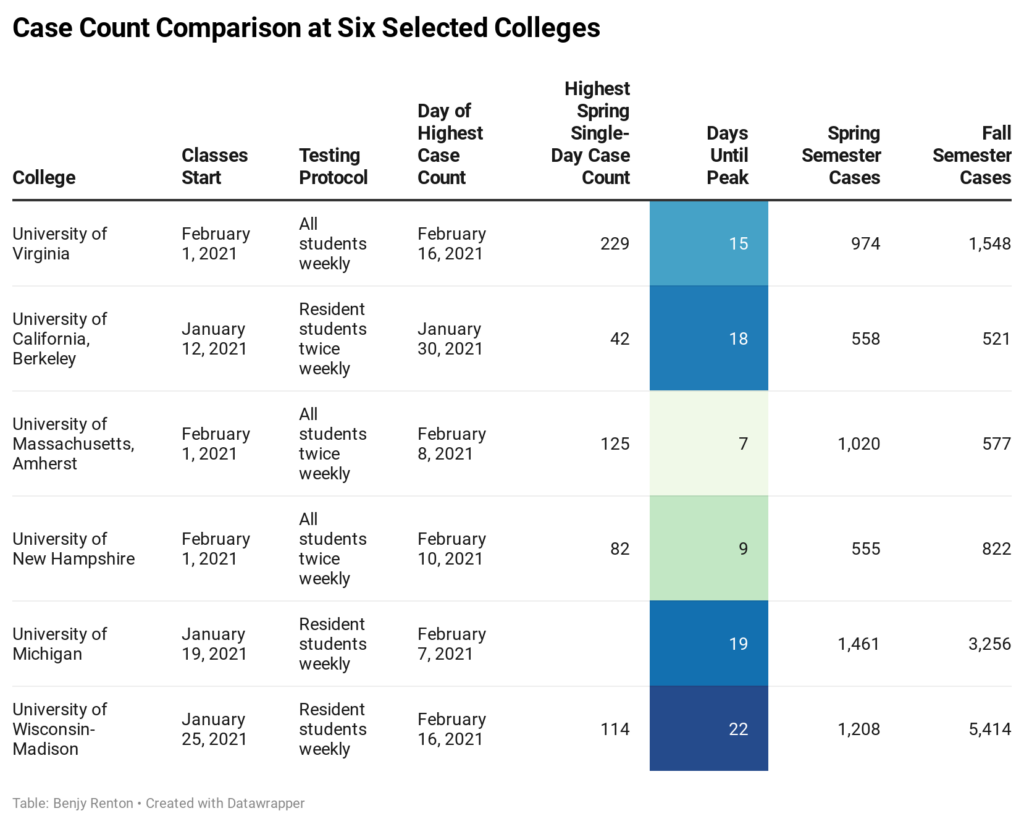
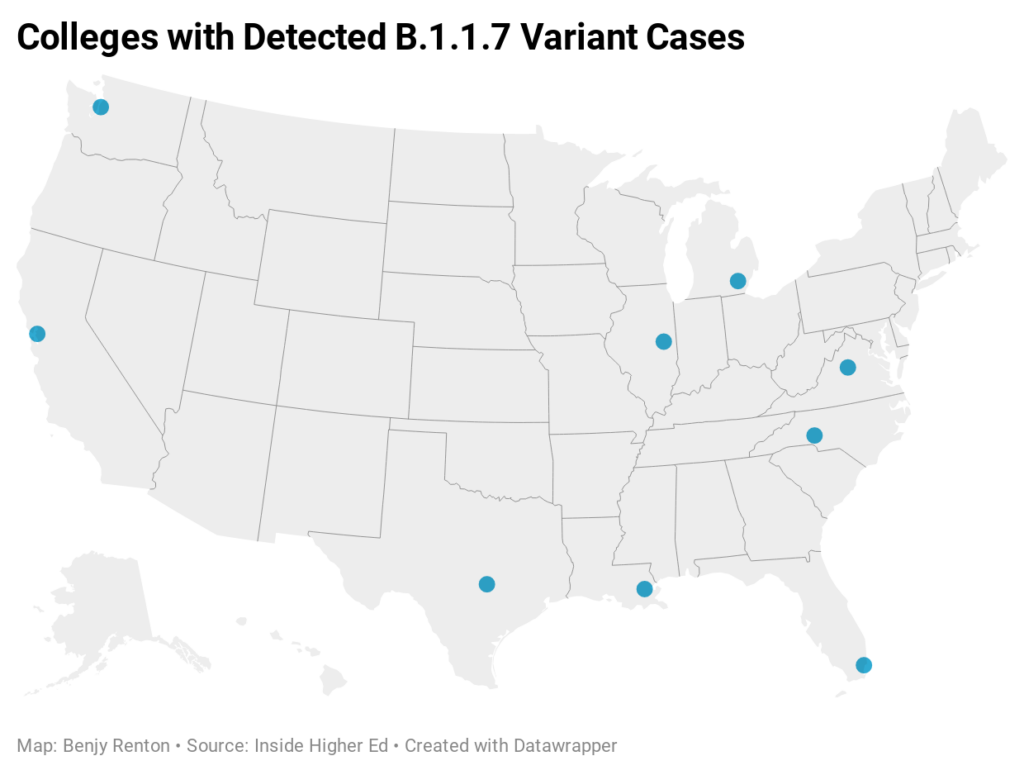
What does this mean? Based on the virus’ incubation period and national transmission, we can assume that cases are imported when students return to campus. However, the vast majority of spread occurs when these imported cases spread to others within the first few days after moving in. An additional factor is variants. According to my count using Inside Higher Ed data, the B.1.1.7 variant has been confirmed on 9 college campuses. 3/6 of the colleges in this analysis have recorded variant cases — exact numbers unknown. I applaud the work of many institutions (including the ones listed here) for ramping up testing compared to the fall — it may be because of this we are “finding” more cases. In summary, the first two weeks are critical to controlling outbreaks (solely relying on arrival testing will not cut it). Colleges should consider a quiet/hibernation/phased reopening for the first few weeks, in addition to conducting multiple layers of arrival testing.
Here is a roundup of this week’s higher ed news:
- Hundreds of students at Rice University rushed to receive last-minute vaccine doses after a power outage put 1,000 doses at risk of spoiling.
- “Lehigh cannot continue to wait for inevitable outbreaks to make changes,” the editorial board at Lehigh University’s student newspaper writes. “Our inability to handle COVID-19 is not only an embarrassment, but serves as a serious hazard to students, professors and the entire Bethlehem community.”
- Reinfections of Covid-19 were confirmed at the University of Wisconsin.
- The Ivy League cancelled its spring sports season, while the NCAA will allow some fans at the Final Four.
- Some college housing workers are requesting to be on the priority list for vaccinations.
- Journalists at the University of Massachusetts-Amherst have been doing superb reporting on the school’s outbreak. A surge in cases overwhelmed the university’s contact tracing team and lack of compliance in quarantine housing has led to student life staff being forced to patrol behavior.
- There have been reports at the University of Virginia and Columbia University of underground parties centered around Greek life.
- One Bowdoin College staff member has been posting TikTok videos providing useful information and encouraging good student behavior.
I wanted to finish the higher ed section underscoring the importance of a multifaceted approach to keeping Covid-19 off college campuses. Many schools have significantly increased testing this semester and my fear is that students will see testing as a panacea. Earlier this week, a technology executive in California apologized for hosting a conference after which two dozen attendees and staff members at the event tested positive for the coronavirus, despite having required frequent testing. “I allowed myself a false (and dangerous) sense of security based on the belief that sequential PCR testing serves as a safety mechanism,” Peter Diamandis wrote, “which I can now tell you is a fallacy.” Yes, testing works. But it’s not enough on its own, especially at colleges.
The Good Stuff
Let’s roll the clips of the good stuff. In my usual tradition, I feature my favorite stories from the week. Here are my Top 10.
- Local news organizations in Texas have been essential to keeping their communities informed throughout the winter storm.
- NASA safely landed a new robotic rover on Mars on Thursday, beginning its most ambitious effort in decades to directly study whether there was ever life on the now barren red planet.
- About 3,500 sea turtles were rescued from the frigid temperatures in Texas.
- The Washington Post published an in-depth report on the history of White House cats. Similarly, CNN published an interactive on all the White House pets in American history.
- Alex Trebek’s TV wardrobe was donated to men who are homeless or leaving jail.
- Apple unveiled a small change to its syringe emoji that removes the drops of blood.
- Opera singers in London are helping Covid-19 patients breathe again.
- In times of crisis, neighbors across Texas are helping each other with housing and food.
- More than 700 people have been keeping digital diaries as part of the Pandemic Journaling Project. The New York Times published some excerpts.
- Trump Hotel employees reveal what it was really like catering to the right-wing elite.
Conclusion
As vaccines continue to roll out and case counts continue to decline, there is a cause for optimism. It is likely that by the summer, many Americans will have access to a vaccine and life may return to resuming some normal activities. However, the variants present a clear and present danger in the next few months. As the weather begins to ramp up, we need to stay ahead of the curve by enhancing genomic sequencing and keeping community transmission down.
And no, Senator Ted Cruz, going to Cancun during a pandemic (never mind during a statewide disaster) is a horrible idea.
I’d like to thank all the student journalists with whom I have the pleasure of working. In the next weeks and months ahead, they will become vital in chronicling their colleges’ paths forward for the spring and beyond. Support their work by reading it.
My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments. And don’t forget to subscribe to the weekly newsletter!
For more instant updates, follow me on Twitter @bhrenton.



3 Comments
Jack O’Connor · February 21, 2021 at 10:18 pm
Just appreciate this every week so much. I look forward to it in my inbox. It’s simply the only spot I know this level of distilled, understandable, sourced, and applicable knowledge.
When COVID got into our family’s house last month, I was able to lean on the well-sourced knowledge from these blogs, and digging into the sources themselves, to offer the best care and advice possible. We were able to take care of everyone and had zero transmissions.
Bless you, stay safe, and let’s keep looking to the future with optimism.
Jack O'Connor · February 23, 2021 at 1:05 pm
Hey Benjy,
I was looking at the Kaiser Health News table you displayed on the effectiveness of N95 mask wearing vs. other mask combinations. I’ve been reaching out to both Lisa Brossaeu as well as the one who made the table and it seems that data comes from a slide in a webinar Mrs. Brosseau presented. Unfortunately, even through this communication I’m not finding the data or study behind this table. In addition, I am skeptical of it inherently due to its symmetry / the fact that the same chances of infection occur regardless of whether the one wearing the mask in the situation is infected or not. I thought masks reduced transmission more when on the infected person, but this table does not show that.
Was wondering if you knew where I could find the data behind it, or if there are other sources/studies that show similar results? I don’t doubt the effectiveness of N95s or masks, I’m just looking for more reliable/sourced data that I can confidently share with my friends.
Where We Stand with Covid-19 — February 26 - Off the Silk Road · February 28, 2021 at 7:33 am
[…] Last week, we discussed the effects of severe weather across the country on vaccinations and examined college outbreaks. This week, we will show why the U.S. is currently at a critical point in the pandemic as a third vaccine is on the horizon. […]
Comments are closed.