Welcome back to Week 28 in my weekly reports analyzing the Covid-19 pandemic and its effects on the country and higher education. For those of you reading this on my blog, Off the Silk Road, I have also launched a newsletter, where these reports can be sent directly to your email each week. Click here to subscribe.
Last week, we painted a disturbing picture of the pandemic with various maps and graphics as we discussed how higher education can prepare for the spring. This week, we will draw attention to the alarming surge happening all throughout the country and look at the latest troubling statistics out of colleges.
A national look
83,757. On Friday the U.S. recorded its highest number of cases in a single day since the pandemic began in January. The following, another 82,668 were recorded.
Late last night, news broke that five people in Vice President Pence’s inner circle tested positive for Covid-19. If the head of the coronavirus task force cannot keep his staff safe, how can the administration possibly keep all Americans safe? We have launched a new tracker which will be updated as the outbreak expands.
It is abundantly clear that the pandemic is accelerating in the U.S., despite what the president says. We are clearly not “rounding the turn.” As our death toll surpasses 223,000 Americans, we have lost the equivalent of six 737s fully loaded crashing every day since March 13. This spread is no longer localized to a specific area; it is omnipresent and hitting rural communities hard.
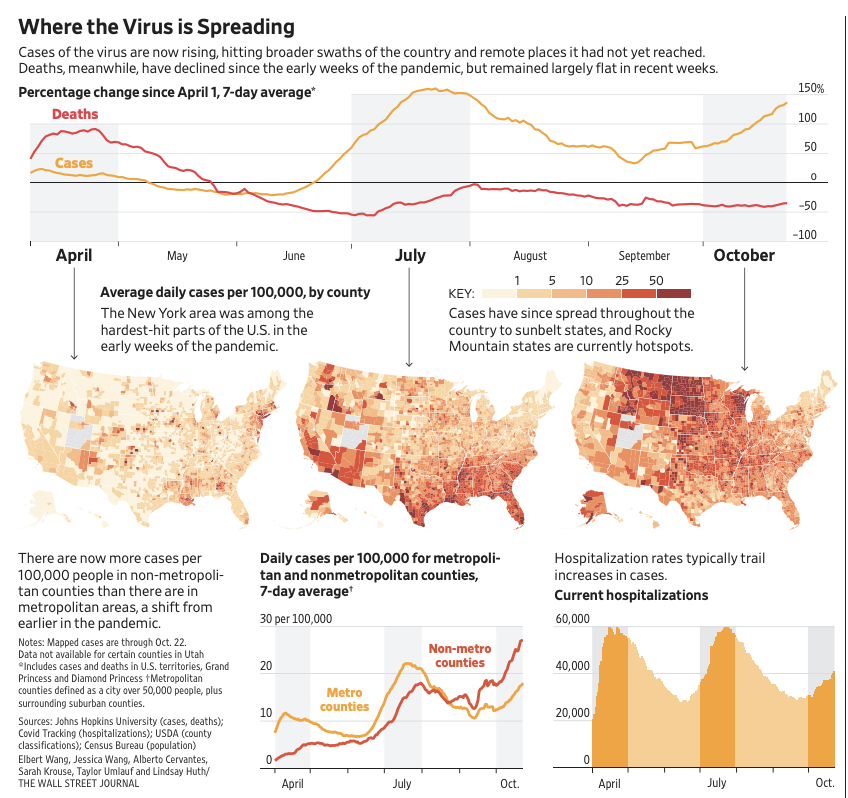
The Atlantic’s COVID Tracking Project broke this surge down into three simultaneous forces:
- An explosion of rural cases, dominated by the Great Plains and the West
- A swing-state surge in the upper Midwest and PA
- A pandemic-fatigue creep in the Northeast and PA again
It is now also clear that the president’s national strategy is to let Americans die. “We’re not going to control the pandemic,” White House chief of staff Mark Meadows admitted on CNN’s State of the Union this morning, touting the administration’s progress on therapeutics and vaccines. Dr. Scott Atlas, the only adviser the president listens to, opposes widespread testing and mask use and the White House is currently sitting on $9 billion of unspent funding for testing. Often promoting “herd immunity” as a strategy, Dr. Scott Atlas is a threat to our nation’s public health. Former CDC Director Dr. Tom Frieden writes, “The route to herd immunity would run through graveyards filled with Americans who did not have to die, because what starts in young adults doesn’t stay in young adults.”
The president has one fatal flaw: he fails to understand that fixing the virus will result in a faster economic recovery. “If you can control the virus, you can get 95% of your life back,” Dr. Ashish Jha, Dean of Brown University’s School of Public Health, said. “In the U.S. and Europe, we wanted to get our lives back, so we acted as if the virus was under control. In Asia, they were not in denial.”
Hospitals across the country are filling up and it will be only a matter of weeks before the country begins to record 100,000 cases per day and the nation will run out of doctors and medical personnel. In the spring, hospitals around the country could reallocate personnel to hotspots; this is no longer possible due to surges everywhere. North Dakota has been so overwhelmed that it has told its residents to do their own contact tracing. In a nursing home in Kansas, all 62 residents tested positive for Covid-19 and 10 died. “Those who deny the scientific realities of the pandemic undermine conditions that allow for rapid and complete reopening,” former New Jersey governor Chris Christie, who was in intensive care after his Covid-19 diagnosis, wrote in a new op-ed in The Wall Street Journal entitled, “I Should Have Worn a Mask.”
“I am lucky to be alive. It could easily have been otherwise.”
Let’s take a look at some numbers of the Covid-19 death toll.
- 223,975 — the official Covid-19 death toll, at the time of writing.
- 299,028 — the excess death count by the CDC from January to October 3.
- 130,000-210,000 — a new Columbia University report shows at least 130,000 and as many as 210,000 lives could have been saved “with earlier policy interventions and more robust federal coordination and leadership.”
It is absolutely terrifying to think about how many deaths could have been avoided and how many Americans are expected to perish in the coming months, as the Institute for Health Metrics and Evaluation’s latest model estimates 385,610 deaths by February 1. In a new study, the modelers estimate that about half of the U.S. population currently wears a mask, and if that number increases to 95%, 130,000 lives can be saved. That would be equivalent to the entire population of Santa Clara, California. A new analysis from Carnegie Mellon University shows a correlation between the percentage of people wearing masks in states and the percentage of people who know someone with Covid-19 symptoms.
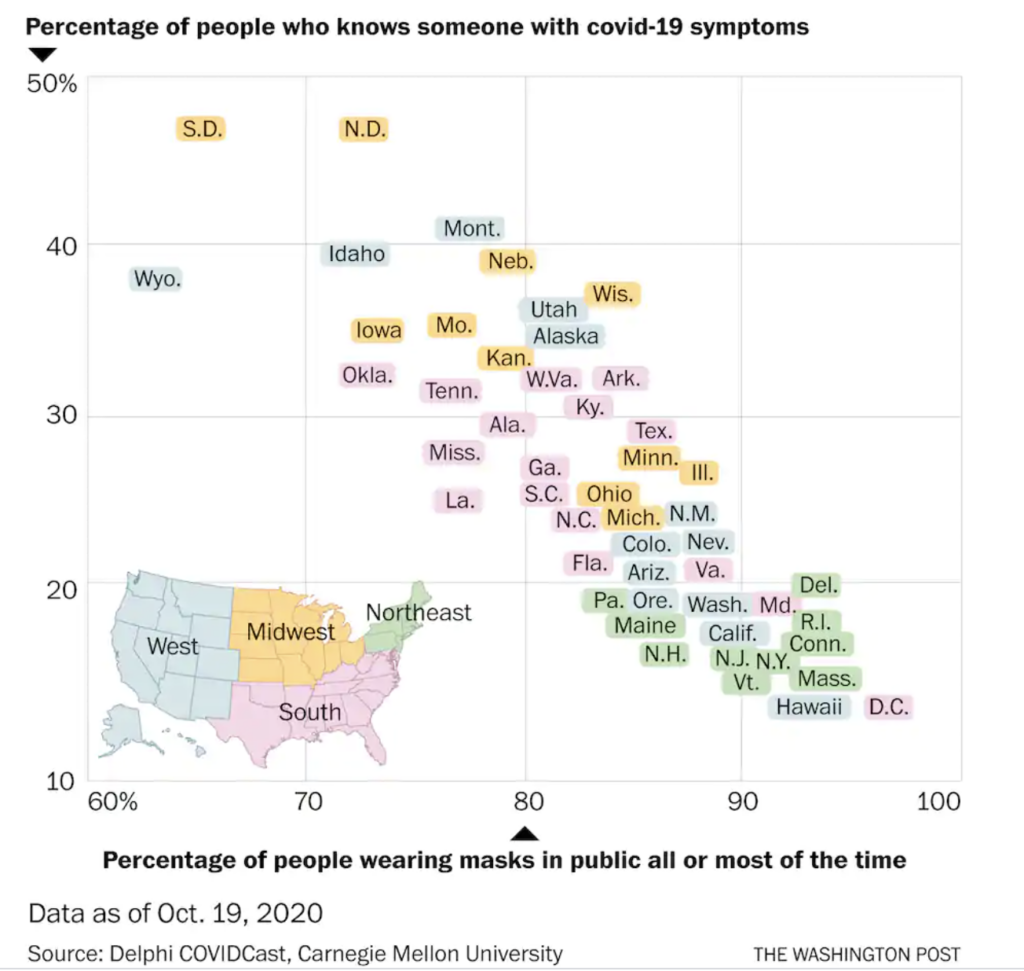
Americans will begin spending more time indoors, and if Alaska points to a possible pattern, cases will only increase. A new survey shows that test wait times have decreased from April to September, but African Americans and Hispanics have longer wait times than those who identify as White. Shockingly, only 56% of positives report being contacted for contact tracing. “We’re not learning to live with it,” former vice president Joe Biden said at the presidential debate this week, referencing President Trump’s remarks. “We’re learning to die with it.” Now the question is: how do you stop Americans from dying? No one in any place in America is currently safe.
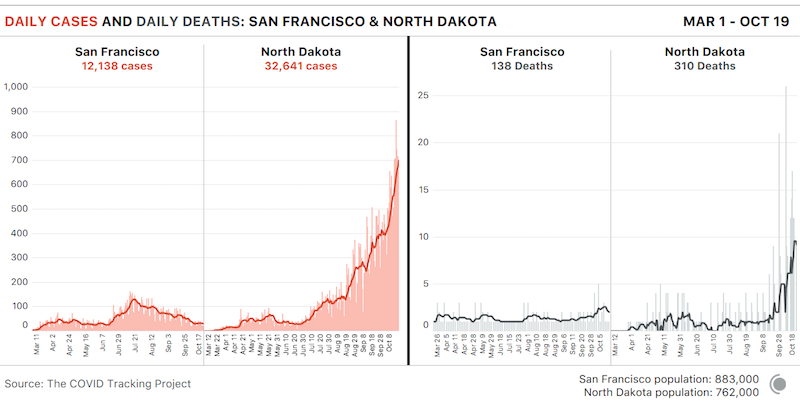
Let’s take a look at some examples of surges throughout the country. The population of North Dakota and San Francisco are quite similar, but a mask mandate imposed in San Francisco in April has kept total cases down to 12,000 and 138 deaths. This week the city recorded 213 new cases. Meanwhile, North Dakota has seen 34,165 cases — including 5,200 just this week — and 323 deaths.
In Ohio, which has seen record high cases this week, we can see a clear spike in cases among 20-29 year olds upon the return of college students. This also comes as cases have increased in all population groups, including the elderly.
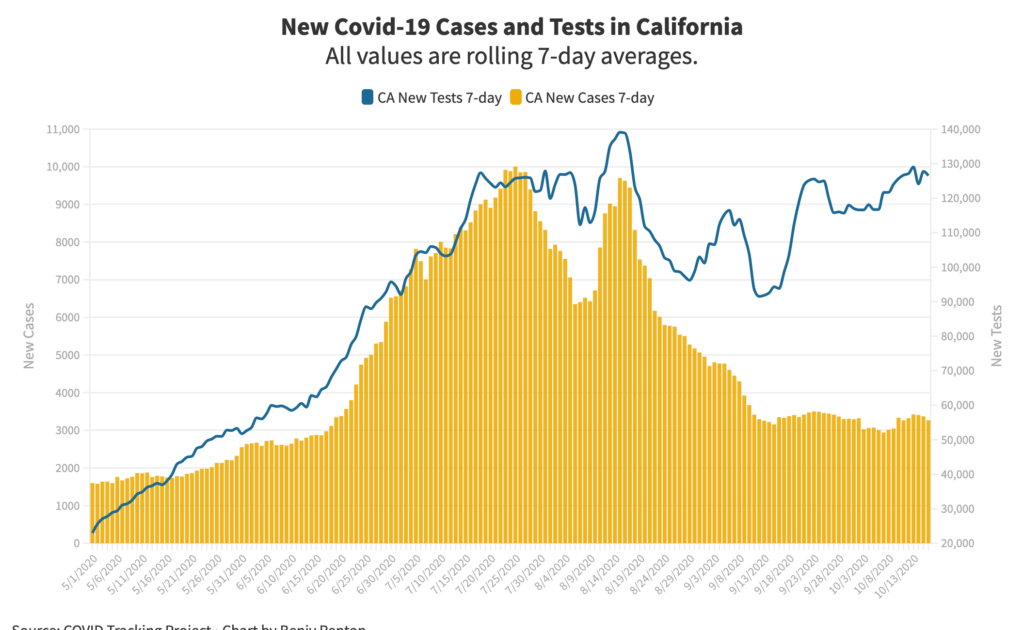
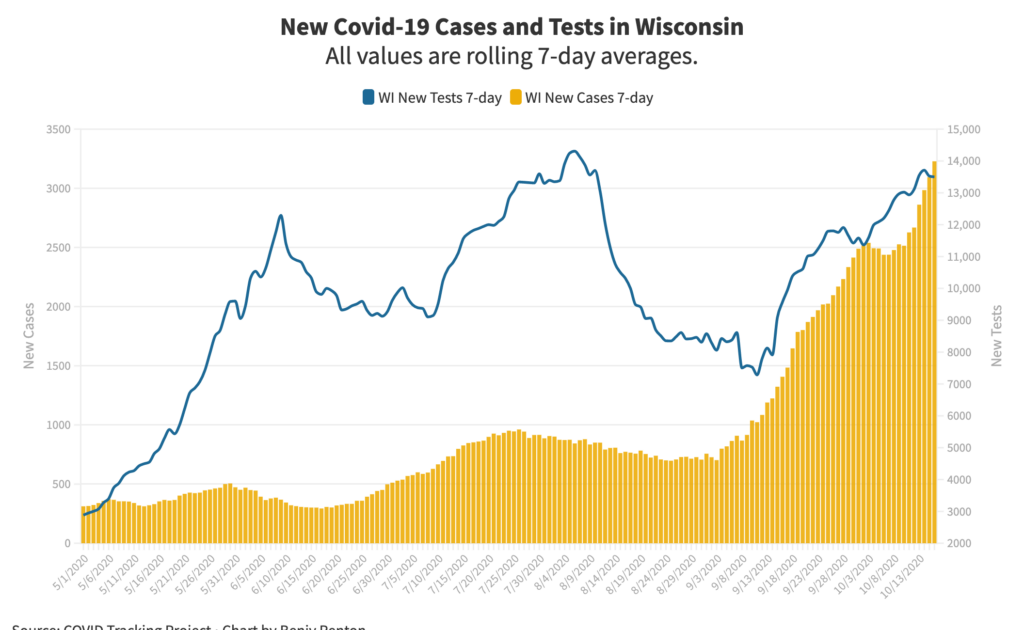
We can also compare trends in Wisconsin and California, which have both seen disturbing surges throughout the pandemic (California’s occurred in the summer; Wisconsin’s is happening now). Normalized for population, Wisconsin’s current surge is much more serious than California’s at the end of the summer. California was able to buck the trend with micro-targeting (on a county level) and a phased reopening, as well as an influx in testing. The graphs below show the new tests (blue) and new cases (yellow) in each state. In response to a surge in June, California was quick to ramp up testing. In contrast, Wisconsin’s daily tests actually decreased in August, leading to a September surge. We also see California is testing a significantly higher portion of their population each day compared to Wisconsin. Testing works!
Let’s take a look at some of the latest scientific developments:
- After a new study at a Vermont correctional facility, where a worker tested positive after multiple short interactions with inmates, the CDC expanded its definition of a close contact. The CDC had previously defined a “close contact” as someone who spent at least 15 consecutive minutes within six feet of a confirmed coronavirus case. The updated guidance now defines a close contact as someone who was within six feet of an infected individual for a total of 15 minutes or more over a 24-hour period.
- A new CDC report shows hospitalized patients with Covid-19 in the Veterans Health Administration had a more than five times higher risk for in-hospital death and increased risk for 17 respiratory and nonrespiratory complications than did hospitalized patients with influenza. Coronavirus is not the flu.
- A new report in the journal Physics of Fluids found that ventilation, spacing, desk shields and hand washing reduced spread in classrooms.
- Testing and tracing work! A CDC report found that in an MLB outbreak, “no secondary transmission during field play between two opposing teams occurred. Interactions outside of game play were the likely source of transmission within the team.”
- In a new study in JAMA of over 5,400 individuals at skilled nursing facilities who were tested positive, 40.6% were asymptomatic.
- One common argument about lockdowns is that they cause an increase in suicides, among other issues. A new preprint published on MedRxiv found that suicides in Massachusetts did not deviate from previous years.
- A new CDC report found that counties with greater social vulnerability were more likely to become areas with rapidly increasing Covid-19 incidence (hotspot counties), especially counties with higher percentages of racial and ethnic minority residents and people living in crowded housing conditions, and in less urban areas.
- An analysis from a Harvard researcher found that the coronavirus has claimed more than 2.5 million years of potential life in the United States since the start of 2020.
- A new piece in Science Magazine on transmission dynamics said that “broad and untargeted interventions may be less effective than expected, whereas interventions targeted at settings conducive to superspreading (such as mass gatherings and hospitals) may have an outsized effect.”
Finally, some updates on vaccines.
- Moderna has finally completed its enrollment in its Phase 3 clinical trials.
- A volunteer in Brazil participating in AstraZeneca’s study died, though we are unsure of further details.
- States have submitted draft vaccination plans to the CDC, including Massachusetts, New York, Michigan and Vermont.
- An FDA vaccine meeting identified some of the issues in distribution, including distrust in government and fear that the vaccine will not work.
- A survey published in JAMA found that “participants were more willing to accept a vaccine if it was more likely to be effective, the effects were to last longer than a single year, and if the Centers for Disease Control and Prevention and The World Health Organization endorsed a vaccine than they would be when compared to a scenario in which President Trump endorsed a vaccine.”
The nation is in an incredibly dangerous place, teetering on the brink of one American testing positive every second. It is up to all of us to follow basic public health practices.
Let’s move on to our discussion of higher education.
Higher education
We begin today’s discussion with a moment of remembrance for University of Dayton student Michael Lang, 18, who passed away on October 22 following a lengthy hospitalization from Covid-19 complications. Our condolences go out to his family and friends.
Each Friday, I update the College Watchlist, which is currently tracking 110,385 total cases at 93 colleges. At the top of my list of cases in the last 7 days are:
- University of Florida – 260
- Clemson University – 243
- Brigham Young University – 156
- Texas Tech University – 151
- Ohio State University – 136
The New York Times’ dataset includes 214,000 cases at 1,600 colleges.
This week, we will take a look at a few new college outbreaks and examine possible community ramifications. The biggest institution to make headlines was the University of Michigan, where county health officials imposed a stay-in-place order amid a spike in cases. “Undergraduate students, both on and off-campus, must stay in their residence unless attending class, accessing dining services or carrying out approved work that cannot be done remotely,” according to the student newspaper. (Voting is allowed, and so is college football.) This is the first instance this fall that a local health department has imposed restrictions on a college; usually the college gets to it first. “People have been going to parties every weekend, they’ve been having parties in the dorms,” one student told The Chronicle of Higher Education’s Mike Vasquez. “Pretty much nothing has been done about it.”
Another school of concern is Texas Tech University, where its surrounding county (Lubbock County) saw a spike in cases after students returned in August. When we compare the university’s weekly cases with that of the county’s, we see less students testing positive through the university but the county’s cases increasing. This comes as the county’s stats show 29% of cases from people aged 20-29, only 20% of the population. The county also has 212 people currently hospitalized.
According to numbers obtained by my colleague Meg Turner at the University of Central Florida’s student newspaper, following a home football game on October 3, student test positivity rate was a whopping 40%. The university has recorded over 1,000 cases since August, a mixture of self-reports and on-campus testing. Although the university randomly selects Greek life for testing, to do ~300 tests per week for a student body of 68,000 (0.4% a week) is pathetic.
On the other side of the spectrum, many schools in the Northeast have seen success in keeping the virus at bay through a partnership with the Broad Institute for testing. When we use New York Times data to compare 88 of the 108 schools vs. 1,400+ in the country, we see significantly lower case counts in schools that use Broad. The results are wildly impressive — colleges that have contracted Broad for testing have an average of 4 cases per 1,000 students, compared to an average of 14.1 cases per 1,000 students of the other 1,300+ schools in the dataset. Are there other factors that contribute to these schools’ successes? Of course — many are in rural areas in the Northeast with low community transmission and have high levels of compliance with health precautions. In the coming weeks I’ll be examining these confounding variables. It’s also worth noting that there are many other testing providers colleges across the country use — Broad is just a noteworthy example as it conducts about 7% of the nation’s total Covid-19 tests each day. Other colleges have in-house labs/facilities, which are beneficial. Here is a map of the colleges in The New York Times’ dataset sized by cumulative case count.
Following are some samples from op-eds and editorials in student newspapers this week, which are always useful for capturing perspectives from students, faculty, staff and local community members.
- “The days have become a structureless blur of breaking news, online meetings, quarantines and, of course, our usual course loads,” editors at the University of South Carolina’s newspaper write as they take a week off publishing for mental health. “While we strongly stand by our commitment to report, fighting burnout and practicing self-care ensures that we will be able to continue.”
- “The pandemic has not reached a statute of limitations, and we cannot slip back into business as usual,” editors at the Stanford Daily write as they push for accessibility and flexibility from faculty. “These are still unprecedented times.”
- “We see your Instagram posts. We see your Snapchat stories. And we’re just wondering: Did you forget that we are living through a pandemic? Did you forget that people are dying?” editors at the Daily Tar Heel at UNC write.
- “Fair treatment is a small price IU must pay for this work,” resident assistants at Indiana University write on their experiences living in dorms.
- “I did not expect to be part of the herd,” Middlebury College student Porter Bowman writes after his semester in Sweden and testing positive for Covid-19 antibodies. “When and if this pandemic reaches an end after months if not years of interruption, death and economic collapse, Sweden will not be standing above the fray.”
- “Target is offering a $5 coupon to anyone who gets a flu vaccine at their pharmacy. Yes, you read that right. FIVE dollars. You know what you can get with five dollars? That’s 4.2 packs of gum. It’s 16 ounces of Haribo gummy bears,” editors at the Daily Tar Heel write as they encourage fellow students to get flu vaccines.
- “When else in our lives will students have the importance of voting impressed on them more deeply than when their University takes concrete steps to make voting and poll-working logistically easier in a time of national crisis?” editors at the Harvard Crimson write as they push for Election Day to be a college holiday.
We finish this week’s discussion with case counts in two Wisconsin counties: Dane County (where UW-Madison is located) and La Crosse County (where UW-La Crosse and Viterbo University are located). This week, The Washington Post ran a story on La Crosse County, “a wildfire of infection that first appeared predominantly in the student-age population, spread throughout the community and ultimately ravaged elderly residents.” In last week’s newsletter, we discussed a preprint which used genomic sequencing to find the same strain of virus through colleges and a nursing home. The county has a population of 118,016, 15% of whom are students at one of these three schools: UW-LAX, Viterbo and Western Technical College. Viterbo’s random asymptomatic screening may have failed to capture many cases before they spread. UW-LAX’s antigen testing for all on-campus students (30%) was helpful, but it’s off-campus spread that’s an issue. We see a clear case spike after the start of classes at the universities, and then a small spike in deaths over a month later.
Here is where age demographics come into play. 18.5% of the county’s population is aged 20-29, but in mid-September this group accounted for 46% of all cases. We also see the beginnings of a possible second “wave,” illustrating the ripple effects through a community.
We have also seen a similar pattern in Dane County, where the University of Wisconsin-Madison is located. Just weeks after classes started, we saw case spikes in the 10-19 age group (likely many freshmen and sophomores, as they live on-campus and are tested frequently). This is also followed by a small spike in hospitalizations.
Without genomic sequencing, it is hard to ascertain directions of transmission and at this point, we cannot make a definite statement of causality between college reopening and increased number of hospitalizations. However, it is a pattern that we must watch on a wider scale, and I look forward to presenting more data in the coming weeks.
So what did we learn from these two counties?
- College outbreaks can and will affect their communities. An idea of a “bubble,” in many cases, is naïve.
- Suspending in-person operations (like UW-LAX did) can slow the spread.
- A “herd immunity” strategy will not work. It will result in deaths.
The Good Stuff
Let’s roll the clips of the good stuff. In my usual tradition, I feature my favorite stories from the week. Here are my Top 10.
- Astronaut Kate Rubins voted from the International Space Station. If she can vote from space, you can at your nearest polling place!
- Despite being from two opposing political parties, the two candidates for Governor of Utah teamed up to shoot a video pledging a peaceful transition of power.
- As the pandemic keeps older poll workers from volunteering, younger women continue a legacy of being on the front lines of elections.
- One doctor in India recorded a now-viral video of him dancing in front of his Covid patients.
- An immersive theater show of “The Great Gatsby” has returned in London, under coronavirus precautions.
- My colleagues at the Brown Daily Herald had an excellent first podcast episode with Dr. Ashish Jha on the latest Covid-19 news.
- A Boston woman went viral for voting at Fenway Park in her Patriots Jersey with her “dunkies.”
- The Daily Princetonian at Princeton University has a fantastic series where they interview kids of professors. This week, a 10-year-old discussed his taekwondo prowess, his mom’s mind-reading abilities and what he misses most about being on campus.
- The Washington Post sent teams of reporters and photographers to six cities — Houston, Albuquerque, Chattanooga, Sarasota, Atlanta and Columbus — to capture how people feel as they wait for their chance to be heard at the voting booth.
- The New York Times teamed up with local news organizations across the country earlier in the year to document the lives of a dozen Americans who found themselves out of work.
Conclusion
As the White House battles a second outbreak, this time around the vice president’s circle, it is incredibly clear that they have abandoned all responsibility to keep Americans safe. The fall “surge” is here in full force and there is no peak in sight. Cases will undoubtedly increase over the next few weeks as more Americans spend time indoors and flaunt basic public health precautions. It will then set off another chain reaction of a spike in hospitalizations and deaths. We return to the question I initially posed at the beginning of the newsletter: how do you stop Americans from dying?
Wear a mask. You can do your part to avoid 130,000 deaths. And vote like your life depends on it, because it does.
I’d like to thank all the student journalists with whom I have the pleasure of working. In the next weeks and months ahead, they will become vital in chronicling their colleges’ paths forward for the fall and beyond. Support their work by reading it.
My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments. And don’t forget to subscribe to the weekly newsletter!
For more instant updates, follow me on Twitter @bhrenton.


