Welcome back to Week 18 in my weekly reports analyzing the Covid-19 pandemic and its effects on the country, higher education and study abroad. For those of you reading this on my blog, Off the Silk Road, I have also launched a newsletter, where these reports can be sent directly to your email each week. Click here to subscribe.
First, a short video on the past 18 weeks and the next steps for the weekly newsletter:
Last week, we discussed a “new phase” of the pandemic as the virus spreads into rural areas and some colleges abandon plans for an on-campus fall semester. This week, we will continue our examination of testing on a nationwide scale, as well as review outbreaks already on college campuses and recent suspensions of football seasons.
There’s a lot of material to go through (as per usual), so let’s get straight to it.
A national look
The theme of this week’s report is “Critical Weeks.”
Time is running out. America’s window of opportunity to beat the virus is narrowing. Here is what we know: models forecast that transmission could increase in the fall and winter, due to more people being indoors, people going back to school and the combination of Covid-19 with the flu season. Cases will likely increase. The issue for us now is to get our case numbers down so we can effectively mitigate transmission and control the burden on our healthcare system. Regional strategies will not work. It is not too late for a national strategy, and if we do not take action, in the words of CDC Director Dr. Robert Redfield, we could be bracing for the “worst fall” that “we’ve ever had.”
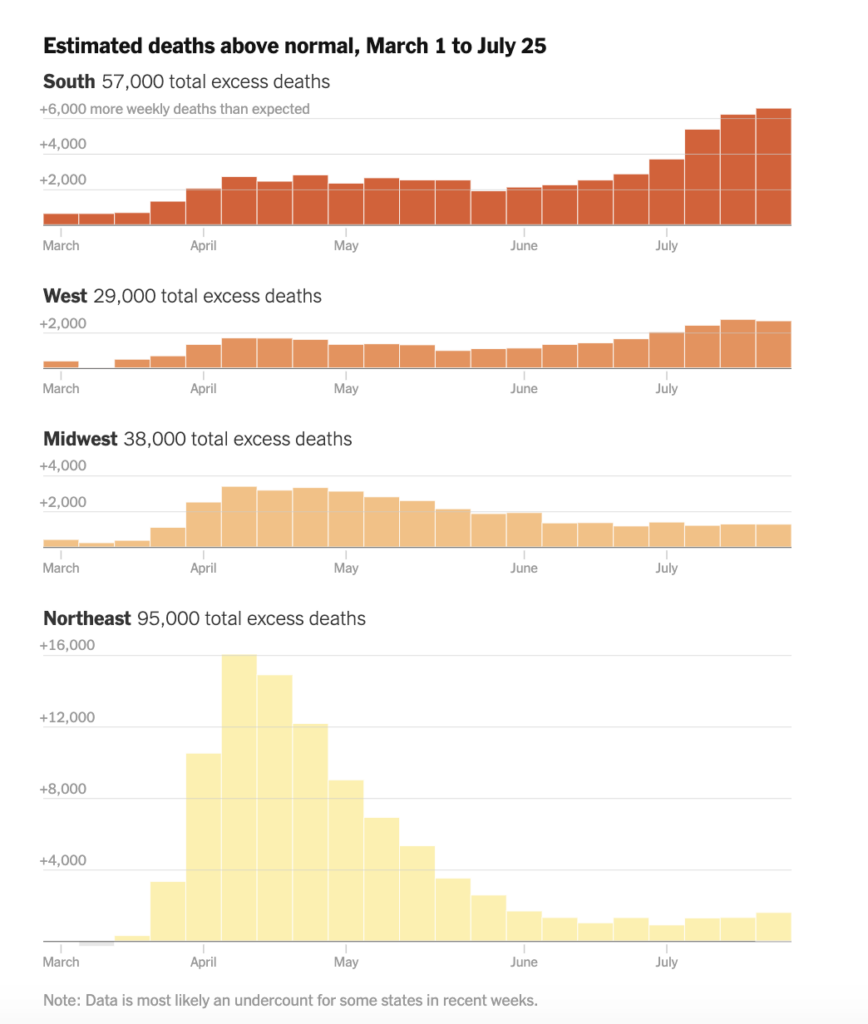
Let’s start with the good news. Cases and hospitals have decreased slightly, to around 56,000 new cases per day and around 46,000 hospitalizations nationwide. The bad news: over 1,000 Americans are losing their lives every day, some days as many as 1,400. The CDC has predicted a total of 189,000 deaths by September 5. Meanwhile, a New York Times analysis has found that the true death toll has already exceeded 200,000 as a result of underreporting from some passing at home, among other reasons.
As some experts call for a national lockdown over the next few weeks, others call for “smarter lockdowns.” Instead of locking down entire cities or states, we should shift to a “household lockdown” model — effectively isolating households with positive cases so that home transmission can be contained and not spread to others. This will help us return to some sort of normalcy while enabling our testing and tracing systems to effectively pinpoint outbreaks.
We received an alarming new report from the American Academy of Pediatrics that nearly 180,000 children have tested positive for Covid-19 in the last month, a 40% increase in child cases. At least 97,000 children tested positive for Covid-19 in the last two weeks of July. According to the CDC, more than 7% of new cases are children. It is particularly disturbing since the number of cases in children keeps increasing, as seen in this graph. There are a few reasons for this: it is possible that children are finally getting tested due to more testing availability and more children are being infected as a result of them being out and about over the summer.
“Trump and many of his top aides talk about the virus not as a contagion that must be controlled through social behavior but rather as a plague that eventually will dissipate on its own,” The Washington Post reports, detailing America’s lost summer. This president has done more for water flow from showers and voter suppression this week than he has to solving the virus problem. “I’m not pleased with how things are going,” Dr. Anthony Fauci said to National Geographic.
If we’re going to solve this problem, we need more testing. On CNN, White House testing czar Admiral Brett Giroir said that “Everything that can possibly be done has been done.” The U.S. is conducting between 700,000 and 800,000 tests per day. The Harvard Global Health Institute estimates we need between 3 and 4 million daily tests, or at least 1 million if we want to have any chance at fighting the virus. Testing seems to be rebounding after decreasing last week. The decrease was extremely odd. We need more testing, not less.
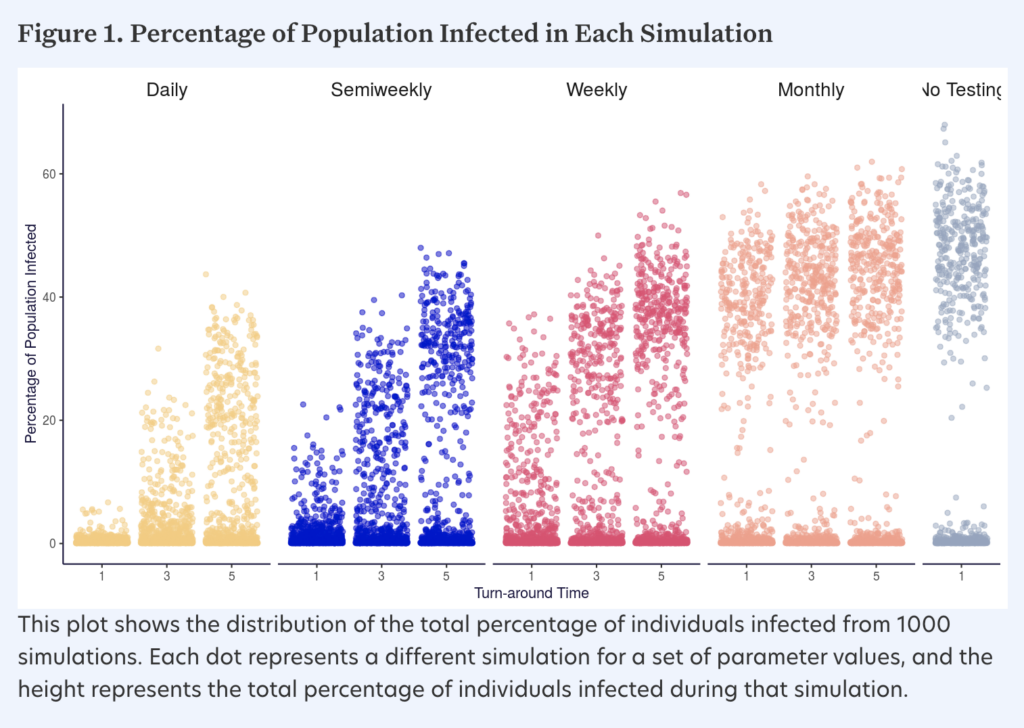
Carl Bergstrom, biologist at the University of Washington, along with his research team, has devised a model that shows the effects of proactive testing with high frequency and rapid turnaround. In his view, testing can be conducted for four purposes: individual health, clearance, surveillance and mitigation. Tests for individual diagnosis need a high sensitivity and specificity — PCR tests are best for this. Tests for clearance would be able to verify that patients are not infectious before a procedure, such as travel or a doctor’s visit. Here, high sensitivity (the ability to detect true positives) is needed, but specificity (the ability to detect true negatives) is less essential. Tests for surveillance help track the spread of the virus within a population. Tests for mitigation are to detect pre-symptomatic or asymptomatic cases in order to isolate and trace contacts before large outbreaks occur. The final two scenarios are best suited for college campuses. The goal in testing for mitigation is to reduce the number of exposure days — how long people who have been exposed are walking around and potentially infecting others. This graph shows the effects of different turnaround times on total infections. Fast turnaround (a day, ideally) is key.
We have seen promising new developments on other forms of testing, which will help reduce the burden on PCR testing (both in terms of resources and lab capacity). E25Bio, a Cambridge, Massachusetts-based biotech startup that develops diagnostic tests for infectious diseases like dengue and Zika, has a new rapid antigen test for Covid-19. This test is similar to a pregnancy test and relies on saliva on a paper strip. While it has not yet received an emergency use authorization from the FDA, rapid antigen tests will be key to solving the testing crisis. LAMP, which stands for loop mediated isothermal amplification, is another way to analyze DNA for the virus and can create a highly scalable solution, as seen in this LamPORE testing assay. One of the more game-changing tests is SalivaDirect, which was developed by researchers at the Yale School of Public Health. This test was just granted an emergency use authorization by the FDA yesterday. Like E25Bio’s test, SalivaDirect analyzes saliva and was developed in conjunction within the NBA. Unlike PCR tests, it does not rely on complex swabs or reagents, which are hard to obtain. The test was found to be “highly sensitive” with “high agreement” in testing outcomes when compared to ordinary nasopharyngeal. The cost of this test to the consumer is around $10, dramatically cheaper than $100 PCR tests. The turnaround time is around 24 hours and the test developers have made the equipment “open source.” Not seeking to profit from this new technology, the test developers want to get the test out to labs to run themselves. This is a landmark accomplishment and I hope that we will see similar tests on the market in the weeks and months to come. We need to flatten the testing curve to reduce strain on our labs and save PCR tests for specific diagnoses. Regulatory approval from the FDA is inhibiting the ability for antigen tests to be easily released to large populations.
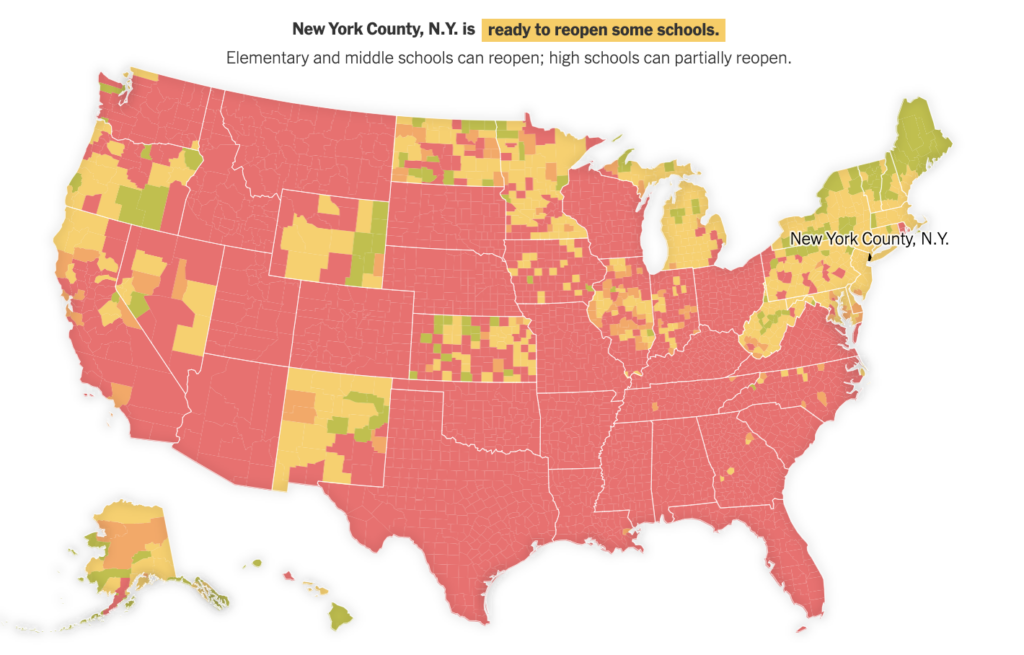
Let’s take a look at K-12 schools and school reopenings. Simply put, some school reopenings in the South are a mess. At least nine cases were reported at North Paulding High School in Georgia and the school’s initial response was to close for only two days. “Disinfecting these schools is like firemen going into a burning house and turning off the stove,” Dr. Rochelle Walensky said. Over 900 people were forced to quarantine at another high school in Georgia after 59 cases were confirmed. That is an average of over 15 contacts per student. The decision to send one’s kids back to school is a complex one and should consider spread in the community and the individual school’s safety precautions. “This was not an easy decision, but one that we believe best respects the science, decreases the risk of further spread and follows the task force criteria,” CNN’s Dr. Sanjay Gupta said of his decision not to send his three kids back to school in Georgia. The White House’s new guidelines for returning to school do not even mention the words “testing” or “tracing,” and are eight simple points which do nothing more but elevate basic hygiene procedures. This comes as survey results published in the Journal of the American Medical Association show that 31% of parents will probably or definitely keep their children home for the fall. “As difficult as distance learning was, returning to the classroom now…would put my home and the homes of millions of low-income kids of color at greater risk of infection,” one high school senior wrote in a New York Times op-ed. Using data that we have previously analyzed from the Harvard Global Health Institute, which uses the number of new cases and test positivity rates in each county, The New York Times has created a useful tool for parents to decide whether or not to send their child back to school. As seen on this map, much of the country would not meet criteria to open schools.
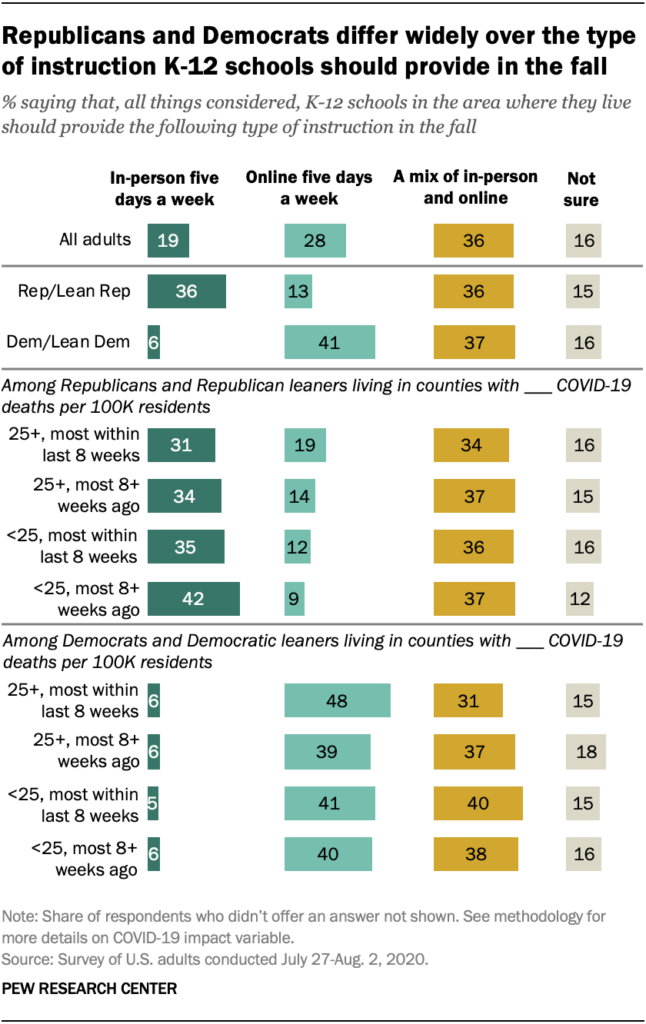
Meanwhile, sending kids back to school is an issue divided largely among political lines.
As usual, more studies have been published and new information is now available to help us better understand Covid-19. Let’s take a look at some of the highlights:
- A widely viewed study published in Science demonstrating how to evaluate face masks showed how simulated respiratory droplets could travel through masks. Researchers found that the fitted N95 mask blocked the most droplets, and a “fleece” such as a gaiter seemed to break down larger droplets into smaller ones. This does not necessarily mean, as some media outlets reported, that they do “more harm than good.” Rather, this study should just serve as a lesson in mask evaluation techniques and more research and trials are needed to evaluate the effectiveness of each type of mask.
- One study from China found that the estimated median of the incubation period is 7.76 days, with 5-10% of people showing symptoms after the recommended 14-day quarantine period.
- We are still learning more about aerosol transmission — one study showed that infectious virus can still remain in the air for up to three hours, though it is unknown how much this contributes to overall transmission from human to human.
- A “mild Covid-19 infection” can have many definitions.
- A study in the American Journal of Pathology, while not randomized and controlled, found that treating patients with convalescent plasma could significantly decrease mortality rates; more research, however, is needed.
- We received long-awaited study results from the Diamond Princess cruise ship, which suffered the first major ship outbreak in February. The attack rate for passengers in single-person cabins or without infected cabinmates was 18% (58/329), compared with 63% (27/43) for those sharing a cabin with an asymptomatic infected cabinmate, and 81% (25/31) for those with a symptomatic infected cabinmate.
- At least 800 people died and 5,800 were admitted to hospital as a result of coronavirus-related misinformation on social media in the first three months of this year.
- A CDC study of 9,000+ Americans shows how the pandemic has affected mental health: 31% had anxiety/depression symptoms, 26% had trauma/stressor-related disorder symptoms, 13% started or increased substance use and 11% seriously considered suicide.
- By some measures, the toll of the Covid-19 surge in New York City this spring resembled that of the 1918 flu pandemic, according to a study described in The New York Times. In March and April 2020, the overall death rate was just 30% lower than during the height of the 1918 pandemic in the city, despite modern medical advances.
- Contact tracing in Guangzhou, China shows that cases had a secondary attack rate of 3.7% — this is the proportion of contacts from confirmed cases that are infected. There was an average of 8.7% contacts per person, and the household attack rate was 10.3%. This can be compared to the healthcare building (hospital) attack rate of 1%. The bottom line is you are more likely to transmit this virus among people you live with instead of interactions in other settings.
- A study published in the Journal of Virological Methods found that anterior nares swabs (the lower nostrils) performed just as well as nasopharyngeal swabs (the upper part of the throat that connects the nose and the mouth).
- A new CDC report shows that 26% of the 3,142 total counties in the U.S. were identified as Covid-19 hotspots (counties meeting specified criteria relating to temporal increases in number of cases and incidence) at some point in the past three months; these counties included 80% of the U.S. population.
- Updated CDC guidelines say that people do not need to test or quarantine within the first three months after infection; people are unlikely to get reinfected in the first 3 months. This was erroneously reported by some media outlets as immunity lasting only three months, which is not true. We don’t know enough.
- T cell immunity could show some long-term infection against future infection with Covid-19. We do not know much about this as the majority of immunity studies focus on antibodies.
Let’s also take a look at developments around the world.
- After over 100 days of no locally transmitted cases, New Zealand detected four new cases, possibly imported through freight. This put the capital city of Auckland into a near lockdown.
- Canadians are concerned about Americans sneaking across the border and infecting them, reporting illegal American visitors.
- Writer Peter Hessler describes his experiences returning to teaching in China after it flattened the coronavirus curve.
- Health and Human Services Secretary Alex Azar visited Taiwan earlier in the week and compared notes on the pandemic.
- A recent rise in coronavirus cases among high school students in South Korea raised the alarm about a bigger risk to school safety.
- Sweden’s chief epidemiologist suggested keeping schools open in a drive for herd immunity.
- Spain is experiencing a second virus wave.
- The pandemic appears to have spared Africa so far. Scientists are struggling to explain why, which could have a connection to blood type.
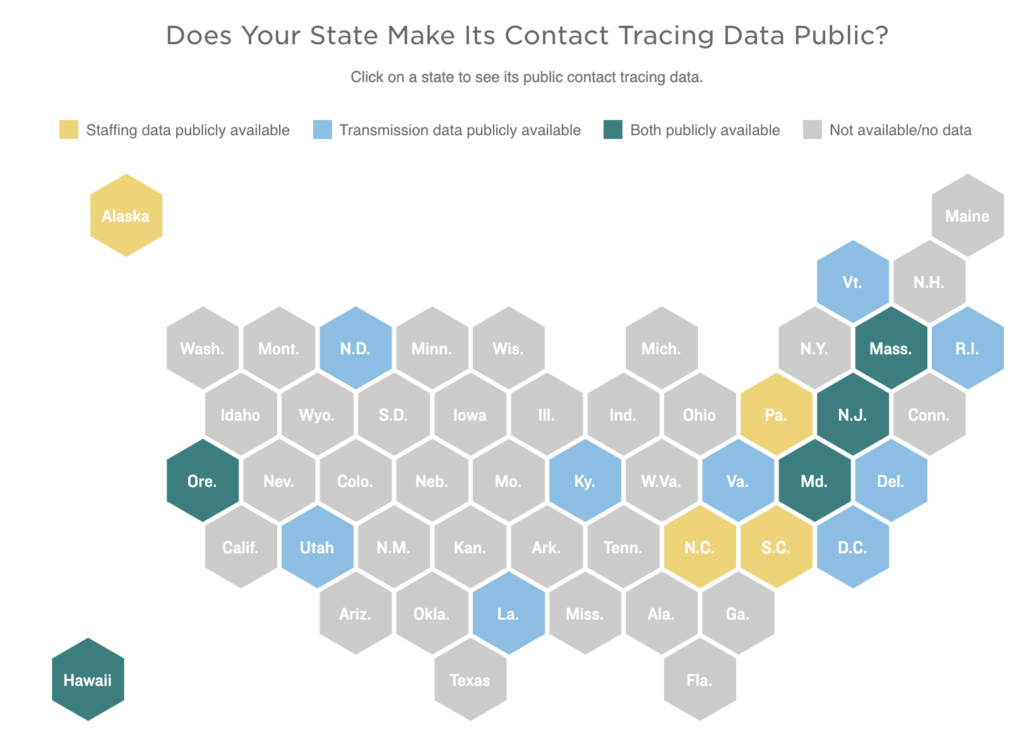
Health experts have warned about the accuracy of the new national hospitalization data recording system, which has been rather inaccurate and unreliable. The vast majority of states are gathering data from their contact tracing programs, but only 14 respondents reported that the data was posted on a government website. We need more transparency when it comes to data to ensure that we have enough contact tracers and that as many cases are being traced as possible. For example, in New Jersey, these data show that public health workers reached only 44% of new cases within 24 hours, and nearly half of those reached refused to provide contacts.
Finally, let’s take a look at some updates on vaccines. Russia’s “approved” vaccine has not undergone Phase 3 clinical trials, nor has data been released, so U.S. health experts question its effectiveness and safety. This is dangerous as public confidence is needed for successful vaccination programs. The Washington Post has released a useful vaccine tracker to understand the 29 vaccines currently in trials worldwide. Results from the Phase 1/2 clinical trials from the Sinopharm vaccine in China showed production of neutralizing antibodies and 15% of participants with mild side effects (pain at the injection site or fever). The U.S. is in the process of creating a coronavirus strain that can be used in possible human challenge trials, which Dr. Fauci has called “Plan C or Plan D.” This would involve deliberately exposing people to a strain of the virus, as opposed to Phase 3 clinical trials which detect if the participants acquire the virus in their daily lives. The director of the National Institutes of Health has said an “October surprise” — a vaccine released just before the election, will not happen.
So where do we go from here? These next few weeks are critical to lower transmission before a potential giant wave resulting from returning to school and work. The American people need to utilize outdoor spaces to help lower transmission and adopt basic public health measures. And no, Mardi Gras should not be held next year.
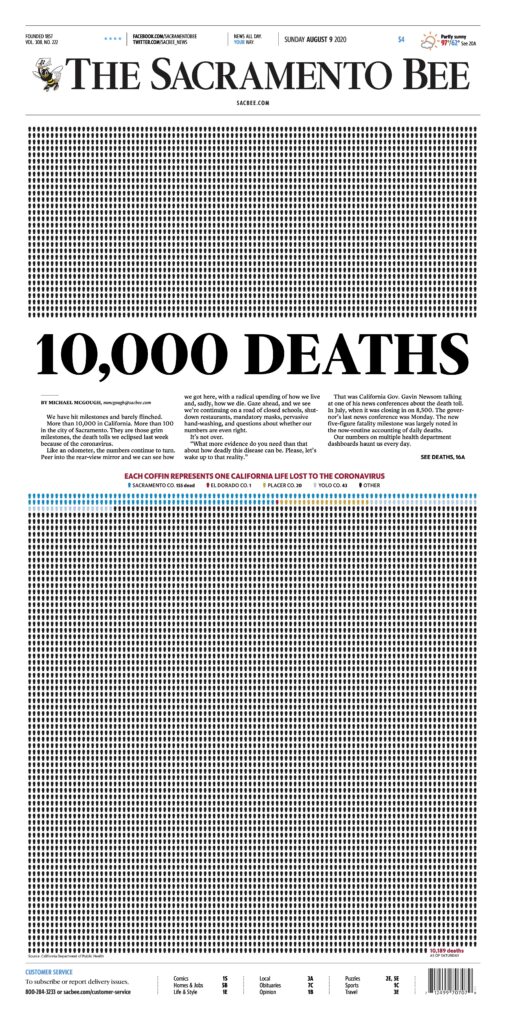
Last Sunday’s front page of The Sacramento Bee marked 10,000 deaths in the state of California. “We have hit milestones and barely flinched,” Mike McGough writes. “Like an odometer, the numbers continue to turn. Peer into the rear-view mirror and we can see how we got here, with a radical ending of how we live, and, sadly, how we die.” Stark images like this help us realize how dire the U.S.’ pandemic situation is.
Having laid down the groundwork on the national scene, let’s review the latest developments in higher ed.
Higher education
According to my Flip Tracker, 153 schools have announced changes or reversals to their fall plans. This number is up from 126 last week.
As I described to Inside Higher Ed’s Emma Whitford, there are geographic trends relating to these changes. Peer institutions in similar geographic areas tend to follow each other’s lead, as seen in some cases in D.C. and New Jersey. Additionally, state and local restrictions play a role; as Los Angeles County prevents colleges from holding fully in-person classes, most schools in the area have shifted to online instruction. One of the stranger, more recent developments is in New Jersey, which now allows institutions of higher education to open in person. This caused Seton Hall and other universities to reverse their previous reversals. Major schools that announced changes this week include Brown University, which pushed back all in-person classes until October 5, and the University of Pennsylvania and Stanford University, which both moved all classes online. This is significant because on April 26, Brown’s president Christina Paxson wrote an op-ed in The New York Times saying that “the reopening of college and university campuses in the fall should be a national priority.” The entire semester at Brown will be remote, if by September 11 cases in Rhode Island have not declined over a 14-day period or the number of students who test positive is “sufficiently low.” Additionally, Columbia University and Barnard College moved to remote instruction just days before some students were due to move in, mostly because of New York’s quarantine restrictions on travelers from a majority of states and the inability of Columbia to accommodate a large number of students quarantining. This makes Cornell the only Ivy League school intending to bring all students back. Some schools in Iowa have delayed the start of classes, not because of the pandemic, but because of devastating derechos that hit the area last week.
College athletics could also push more schools to reconsider fall plans as the Big Ten and Pac-12 cancelled college football (much to President Trump’s dismay). For the conferences that have decided to continue with football, some health experts are worried. “We have a serious problem,” Dr. Carlos del Rio, who advises the NCAA, said. “I feel like the Titanic: we have hit the iceberg and we’re trying to make decisions of when the band should play.”
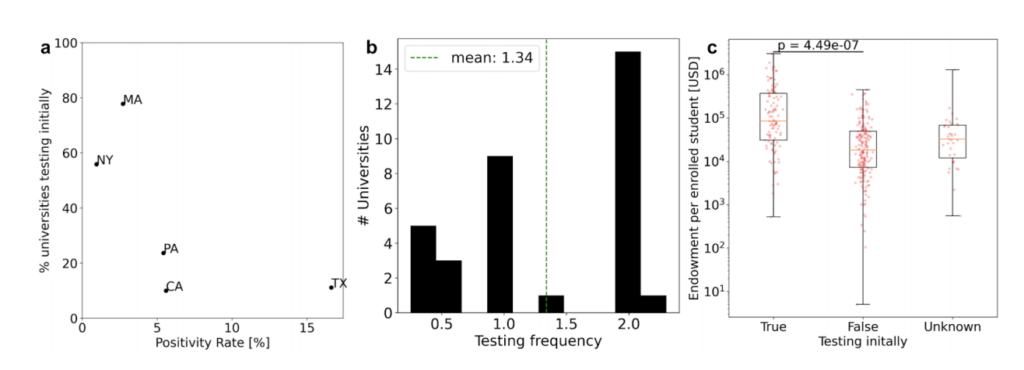
We have long discussed the importance of testing as a component of colleges’ reopening plans. A new analysis of 1,226 higher education institutions in the U.S. conducted by Caltech researchers, a Johns Hopkins doctor and myself found markedly heterogeneous strategies among colleges. Here are some of our key findings in a preprint published on MedRxiv:
- 54% of universities are performing or facilitating some form of Covid-19 testing. Only 27% of colleges are performing initial re-entry testing at least for undergraduates, while an even smaller percentage, 20%, plan to test their communities regularly to some extent.
- In the five states with the most universities (MA, NY, PA, CA, TX) and for which we had extensive data, we find that states with the highest Covid-19 test positivity rate plan for the least amount of initial testing of students returning to campus (Figure 1a).
- However, not all colleges are planning to regularly screen their communities, and even those who do display high variability in the frequency with which they plan to test (Figure 1b).
- Universities with larger endowments are more likely to plan for testing than universities with smaller endowments (Figure 1c).
- Universities that will not provide testing, perhaps due to cost or other considerations, are in some cases offering bizarre rationales. At Newberry College in South Carolina, authorities claim that “testing is not required because the tests available at this time cannot provide assurance that someone will not become sick after the test is performed.”
It’s simple. Colleges should not reopen if they fail to conduct widespread testing of all students on arrival and regular testing throughout the semester. We will discuss the results of testing failures in a bit.
Each week, we take a moment to acknowledge the wackier elements of colleges’ reopening plans, also known as the College RidicuList.
- Boston University has filed a trademark application for a campaign called “F*CK IT WON’T CUT IT” for “promoting awareness of safe and smart actions and behaviors for college students in a Covid-19 environment.”
- Boston University (and some other schools, including the University of Kansas, for that matter) will not notify faculty if students in their class test positive. Their reasoning? One source compared a classroom to a grocery store, questioning if others in the store would be notified. (Well yeah, but you don’t sit in grocery stores for hours at a time.)
- An ongoing discussion that took place before the pandemic resulted in Boston University posting a policy of awarding posthumous degrees in June, which their student newspaper reported this week. According to one professor, the timing of this release was “very unfortunate.”
- Seton Hall University’s gym is an example of “social fitnessing.”
- How is quarantine at Syracuse University going? According to my reporting from my college Abby Weiss, administrators, who previously described quarantine as a “minimum-security prison, said this: “Each pod has two hours of designated ‘outside time’ every day, which is double the amount of time students had during the first week of quarantine.”
- Despite all the research and models advocating for regular surveillance testing, here’s what the president of the University of Michigan had to say: “This notion that a university at the scale of Michigan can test everybody a couple of times a week or every day, right now, that’s science fiction.” (This would be an incredibly dumb science fiction novel.)
- While not implementing a surveillance testing plan, Southern Methodist University is putting their students who test positive in “wellness pods.” (They actually look quite nice.)


When teaching this fall, various instructors have reiterated the need to create virtual communities — enabling students to have smaller discussions and informal meet-ups online. We expect to hear more tips on teaching during a pandemic as more faculty return to the classroom.
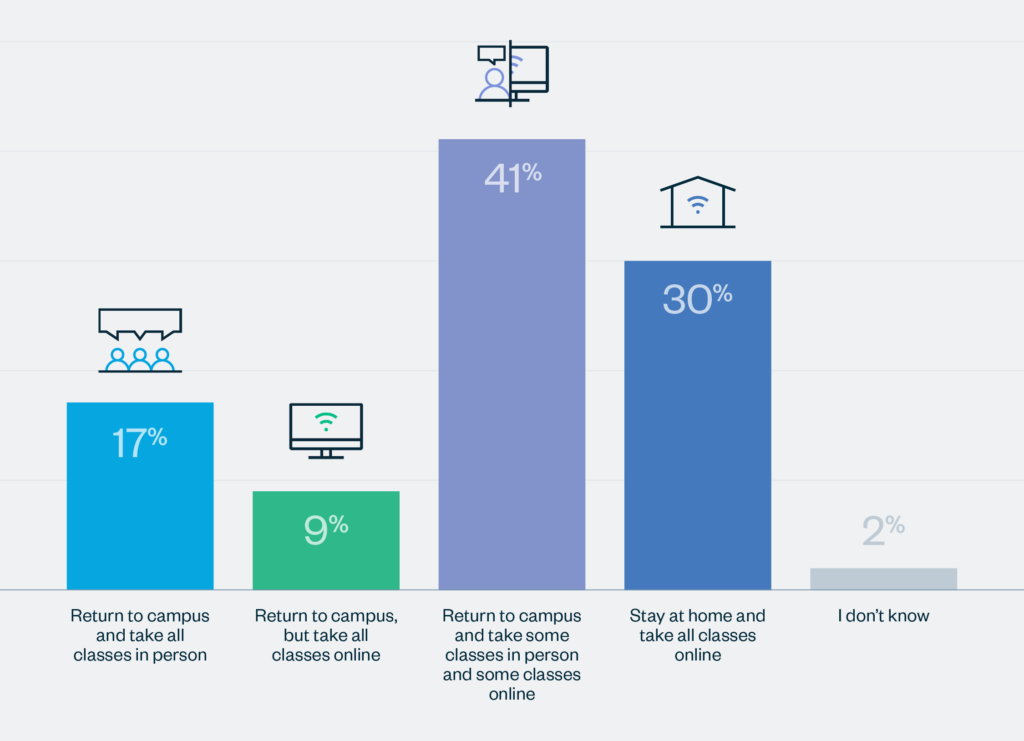
As some students are being compelled to sign liability waivers before they arrive on campus, a new survey from Simpson Scarborough shows updated opinions of college students nationwide.
- 40% of incoming freshmen say it is likely/highly likely they will change their mind about the school they have chosen to attend this fall.
- Students whose school is not reopening for in-person instruction in the fall are more supportive of their institution’s decision.
- Only 17% of returning students express a desire for full-time in-person instruction; 30% would rather stay home and take courses online.
The pandemic is a crisis of communication in higher ed. Colleges must ensure they clearly and concisely convey to their communities exactly what students/faculty/staff must do before they return to campus (a checklist would be helpful). An overload of information is futile.
For those students who have returned to campus for orientation, they are greeted with 10,000 gallons of hand sanitizer and 50,000 social distancing signs, in the case of the University of Notre Dame. Others are faced with virtual orientations, as my colleague Elin Johnson at The Chronicle of Higher Education reports. Student newspapers also face unique challenges — I have developed a set of guidelines in consultation with editors nationwide to provide ideas, support and recommendations for newspaper operations in the fall. We welcome adoption by college newspapers and feedback.
Here are some samples from op-eds and editorials in student newspapers this week, which are always useful for capturing perspectives from students, faculty, staff and local community members.
- “To force students, faculty and staff into shared spaces designed for proximity and flow is dangerous,” one professor at Syracuse University, who contracted Covid-19 earlier this spring, wrote. “To place the responsibility of containing the virus on our students is cruel and misguided.”
- “If I was a senior administrator, I could not open a campus knowing that it was going to kill somebody,” one anonymous faculty member said to Inside Higher Ed. “How anybody could have the dissonance to not put together the direct causality of opening the campus and killing somebody or the willful stupidity to deny culpability when it will happen is mind-boggling.”
- “I know that if I go back I’m going to be undersupported and just not cared for, which I never experienced at Cornell,” one student said. “This is the first time it’s very clear that’s the case.”
- “Vague statements do not reassure students,” one Boston University faculty member said. “They confuse, obfuscate and lessen students’ trust in the administration.”
- “I feel like at this point, I’m kind of just numb to all the out-of-nowhere changes that admin keeps throwing at us,” one Georgetown University student said, demonstrating the potential dissatisfaction among students when a university shifts to remote instruction at the last minute.
- “Many educational institutions with protocols as carefully developed as Middlebury’s have already seen how quickly local epidemics can develop and have wisely switched to all online classes.…We urge Middlebury College to do the same,” a group of current and former Middlebury College employees wrote in the Addison Independent.
- Boston University philosophy professor Daniel Star argues that students will be dissatisfied with their face-to-face courses. “The crucial question is: Why should we think such preferences will not shift substantially once students experience socially distanced, mask-to-mask classes?” he writes in Inside Higher Ed.
- “UNC has always valued profits over people, so why would they stop now?” the editorial board of the Daily Tar Heel, the student newspaper at the University of North Carolina, writes, pushing for more transparency on an institutional level.
- “I shouldn’t have to sacrifice my classes of choice when an able-bodied student gets to go into class,” one student said to USA TODAY, illustrating the concerns brought about by high-risk students.
- We have previously discussed Cornell University’s reasons for reopening; the school argued that not reopening would cause many students to come to the local community anyway and would not be under a robust testing program. “We also must acknowledge that the central paradox of their plans for this semester is generating chaos,” one student writes.
- “We deserve more,” one student at the University of Texas at Austin writes. “We deserve to get an education without worrying the next day could be our last. We should not be reduced to statistics in Travis County’s records. We need UT to put its community members first, even if that means closing campus.”
- While I personally spend very little time on the wild world of Reddit, USA TODAY higher ed reporter Chris Quintana found this quandary raised by a UT student. “So I’m a freshman that will be living on campus and I completely understand why they’re doing this obviously, but with literally EVERYTHING in longhorn welcome week being moved online and like no events or anything happening in person, will there be anything like fun to do at all?” one student asks.
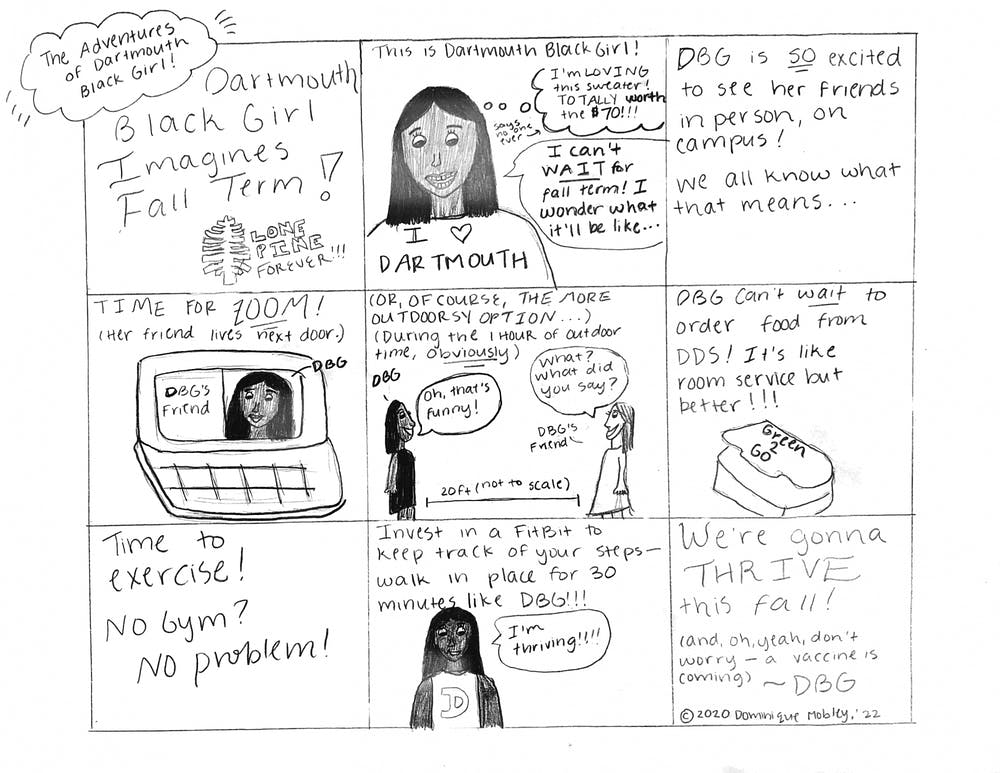
- A Dartmouth College student drew a cartoon of what “thriving” on campus this fall will look like to her.
During the pandemic, colleges are facing simultaneous crises of trust and mental health. “It’s just too much of a risk, and personally, I can just see it going downhill really fast,” one student at the University of Arizona told my colleague Alison Berg at The Chronicle. “I don’t want to move there and then be sent back home.” Some students think being on campus is worth it. “It’s indicative of what being on campus this fall means: a constant push and pull between normalcy and ever-present risk,” The Chronicle’s Lindsay Ellis reports from the University of Kentucky.
Let’s talk about virtual spread. Colleges must monitor two types of spread for monitoring outbreaks this fall: college spread and community spread. Think of it as like peanut butter and jelly. They go together. Therefore, just as it would be plausible for students to evacuate a college as a result of an outbreak on campus, we must prepare for the possibility of an evacuation due to rising cases in the surrounding community. For colleges that open in the fall, they must commit to a level of transparency that includes reporting confirmed cases, number of tests and test positivity rate regularly. These metrics that we use on a nationwide scale must be reported as soon as cases are detected, not weekly.
This brings us to a short analysis of two major outbreaks we have seen this week on college campuses: the University of Notre Dame and the University of North Carolina. Notre Dame has seen 44 new cases in the past few days, many resulting from an off-campus party, as reported by my colleague and recent Notre Dame graduate Kelli Smith. The university, which sent tests to students prior to arrival, saw over 99% of them come back negative. However, Notre Dame did not test all students on arrival, nor do they intend to conduct regular testing for non-athletes during the semester (the university has conducted the vast majority of tests this week on football players). This is a fatal flaw (it’s almost as if science and modeling are right!). Already, the school has begun to blame their students for not respecting guidelines, when I would argue much of their flaws lie in an institutional failure to protect its students. “University spokesman Paul Browne said the increase in cases was a reminder that its coronavirus plan would work only with total cooperation from students,” according to a report in the South Bend Tribune. At the University of North Carolina, which did not test all students on arrival, nor does it intend to conduct regular surveillance testing, three clusters have already emerged in the first five days of classes, one stemming from a fraternity house (a cluster is defined as five or more cases). However, the school will not release the exact case numbers, hiding behind FERPA laws, as reported by my colleagues Praveena Somasundaram and Maddie Ellis. Sean Tierney, Associate Commissioner for Policy and Research at the Indiana Commission for Higher Education (CHE), says that “it’ll get messy.” These two outbreaks are a result of a failure to construct a solid testing plan. We will continue to monitor these two outbreaks, as well as many more, as the situations develop.
Study abroad and international travel
A few updates:
- International students who remained in college towns over the spring and summer were integral to the local economy, as reported by Bloomberg’s Janet Lorin.
- Trump’s impending “ban” on WeChat could have huge implications for Chinese students studying in the U.S. Many feel “unwanted” in the U.S.
- The University of California, Berkeley is the first school, by my count, to suspend study abroad programs for spring 2021.
The Good Stuff
Let’s roll the clips of the good stuff. In my usual tradition, I feature my favorite stories from the week. Here are my Top 11.
- Kaiser Health Network and The Guardian pay tribute to the 922 healthcare workers whose lives were lost to Covid-19 through a series of profiles.
- Stir-crazy travelers are ordering airline food to replicate the in-flight experience.
- Joe Biden’s pick of Kamala Harris as his running mate shocks and excites SNL’s Maya Rudolph. Think Tina Fey as Sarah Palin.
- A voter showed up to a polling place in Vermont on horseback.
- One Jewish museum has seen sales of a “Yo Semite” shirt skyrocket.
- Moving an elephant 1,700 miles from Argentina to Brazil during a pandemic is not as easy as you might think.
- The staff at the Yale Daily News produced a phenomenal first-year issue.
- The Washington Post Magazine ran a series of portraits of frontline workers through a 19th century lens.
- After an op-ed in the Chronicle about faculty curating a zoom backdrop for their courses this fall, one professor showed how he looks “professional.”
- Mei Xiang, the female giant panda at the National Zoo in Washington, may be pregnant.
- A church priest parodies “You’ll Be Back” from Hamilton.”Our worship’s online, but Facebook and YouTube can’t give you the Bread and the Wine. You’ll be back, wait and see, just remember how it used to be…”
Conclusion
The United States is at a crossroads, and these next few weeks are critical to prevent us from facing the worst fall and winter in public health history. We must harness the power of all Americans to suppress transmission going into the fall. Late summer vacations, schools reopening and colleges with students on campus will all contribute to viral spread. It is our job to ensure that we break as many transmission chains as effectively as possible. Testing, tracing, social distancing and mask wearing are our best tools to do this.
As I mentioned in my opening video, going forward, I will be phasing out these long-form reports due to commitments relating to the start of the academic year. However, my reporting will continue and you can follow me on Twitter for the latest updates. Depending on the progression of the pandemic nationally and at colleges across the country, I expect to continue this email newsletter in some form over the coming months, possibly writing a weekly briefing with science, world and vaccine updates, as well as college outbreak developments. I will be in touch shortly as to how this coverage will proceed. I always welcome your feedback as we fight this pandemic together.
Finally, I would like to thank the doctors, scientists and journalists whose materials are integral to each week’s overview of the pandemic. I’d also like to thank all the student journalists with whom I have the pleasure of working, with special thanks to the team at the Colorado College Covid-19 Reporting Project. In the next weeks and months ahead, they will become ever more important in chronicling their colleges’ paths forward for the fall and beyond. Support their work by reading it.
My best to all for good health.
Like what you see? Don’t like what you see? Want to see more of something? Want to see less of something? Let me know in the comments. And don’t forget to subscribe to the weekly newsletter!
For more instant updates, follow me on Twitter @bhrenton.


